
Peripheral-nerve rerouting is an exciting surgical
procedure that has considerable potential for restoring significant
function after spinal cord injury (SCI). Basically, with this procedure,
peripheral nerves (i.e., those outside of the spinal cord and brain)
emanating from the cord above the injury site are surgically rerouted
and connected to those below the injury site. This reestablishes a functional neuronal connection from
the brain to previously dormant muscle or sensory systems.
injury site. This reestablishes a functional neuronal connection from
the brain to previously dormant muscle or sensory systems.
A key force behind developing this procedure into a
real-world SCI therapy has been Dr. Shaocheng Zhang, of Changhai Hospital, Shanghai, China. Because he has treated
over a 100 people with SCI, he has made routine a seemingly challenging
neurosurgical procedure. In addition to Zhang’s work, Dr. Giorgio
Brunelli, University of Brescia, Italy has greatly contributed to
developing the procedure.
After I met Zhang at a World
Health Organization (WHO) SCI conference, he invited me to Shanghai
last December to become the first American to observe firsthand his
peripheral-nerve-rerouting surgery. Because his hospital, Shanghai’s
largest, is military affiliated, this invitation to a Paralyzed Veterans
of America (PVA) representative clearly was a bridge-building, goodwill
gesture. It would certainly be a promising sign for the future if
military-affiliated organizations from two countries that have had
historically some animosity could work together to find solutions for a
problem that bows to no flag or political system
East Meets West:
An impressively modern city with 16-million
residents, Shanghai is located near the juncture of the Yangtze River
and the East China Sea. As China enters the World Trade Organization,
Shanghai seems destined to reclaim its historical role as the
country’s most international city.
Its downtown skyline - with the world’s third tallest
skyscraper and an even-taller, space-needle-like tower - rivals that of
virtually any city.
Although few residents spoke English, its presence
was everywhere. For example, many road, building, and billboard signs
were in English; police cars were prominently labeled with the word
“police”; airplane and train schedules were announced in English;
Christmas carols were piped-in at the ubiquitous, familiar fast-food
restaurants; and rock, rap, and jazz music was played on the radio.
Considerable hospitality and friendship were
extended to me, including much sympathy for the World Trade Center
terrorist attack. Overall, there seemed to be a sincere desire to move
into the twenty-first century as friends of America, not adversaries,
and to work together for mutually beneficial economic growth.
Procedure:
 Unlike
spinal cord nerves, peripheral nerves have considerable regenerative
potential and the ability to establish new neuronal connections.
Building upon these capabilities, Zhang surgically reroutes and
connects a peripheral nerve that emanates from the spinal cord above the
point of injury to nerves or nerve roots below the injury. Hence, a
viable neuronal connection from the brain to the previously
paralysis-affected body area is created, restoring some function.
Unlike
spinal cord nerves, peripheral nerves have considerable regenerative
potential and the ability to establish new neuronal connections.
Building upon these capabilities, Zhang surgically reroutes and
connects a peripheral nerve that emanates from the spinal cord above the
point of injury to nerves or nerve roots below the injury. Hence, a
viable neuronal connection from the brain to the previously
paralysis-affected body area is created, restoring some function.
The nature of the restored function depends upon
the specific functions that the target nerves serve (e.g., leg muscle
function, bladder and bowel control, sensation, etc). For example, the
rerouted nerve could be connected to a nerve that controls urination, or
it could be reconnected to nerve that controls upper leg muscles.
Alternatively, if the rerouted nerve is connected
to a general nerve root system, function in the overall physical area
controlled by this system will be restored. One surgical rerouting
designed to restore a specific function does not preclude a future
rerouting to restore a different function. (Because this article
extensively refers to different spinal cord and dermatome sensation
levels, readers are encouraged to consult the illustrations for
reference).
Many possible rerouting arrangements exist. Zhang
commonly reroutes one of the intercostal nerv es
that lead from the spinal cord around each rib to the sternum. If the
intercostal nerve is not long enough to reach the target nerve site
below the injury level, a segment of the sural nerve (isolated from the
calf) is attached to the intercostal nerve.
es
that lead from the spinal cord around each rib to the sternum. If the
intercostal nerve is not long enough to reach the target nerve site
below the injury level, a segment of the sural nerve (isolated from the
calf) is attached to the intercostal nerve.
If the injury site is above the thoracic area where
the intercostal nerves originate, other peripheral nerves can be
selected. For example, in several cases, Zhang has rerouted the ulnar
nerve, which leads down to the wrist originating from the C8-T1 spinal
cord region, a procedure Italy’s Brunelli has also used.
In addition to the intercostal and ulnar nerves,
peripheral-nerve-rerouting options can restore function for virtually
any level of injury. For example, in high-level injuries, functional
peripheral nerves above the injury site (e.g .,
cervical plexus nerve branches originating from the higher cervical
regions) can be connected to nearby dysfunctional nerves below the
injury site (e.g., brachial plexus nerves originating from the lower
cervical regions), potentially restoring respiratory ability to a
previously ventilator-dependent quadriplegic.
.,
cervical plexus nerve branches originating from the higher cervical
regions) can be connected to nearby dysfunctional nerves below the
injury site (e.g., brachial plexus nerves originating from the lower
cervical regions), potentially restoring respiratory ability to a
previously ventilator-dependent quadriplegic.
Zhang’s patients have lost little function in the
original area served by the donor nerve because of nerve redundancy, the
availability of multiple nerve branches, or the creation of alternative
connections. For example, rerouting one of the many rib-associated,
intercostal nerves will result in little functional loss. In the case of
ulnar nerve rerouting, alternative nerve connections can be created to
the hand and wrist.
Although improvement in some cases is quickly
apparent, restored function will gradually accrue over 12-18 months
depending upon the specific surgical complexity.
While the procedure isn’t precluded for older
patients, younger patients with greater inherent regenerative potential
often benefit more from peripheral nerve rerouting.
In addition, as more time passes after injury, the surgery may
become less feasible, especially for lower-level injuries.
In spite of intimidating neuroanatomical
terminology, peripheral-nerve rerouting is conceptually relatively easy
to understand. For example, visualize a house in which the power to the
back bedroom is lost (i.e., area below the injury) due to a burned-out
master electrical cable (i.e. the spinal cord injury). Instead of fixing
the master cable, you disconnect the wire that powers the living-room
television (i.e., a nerve to the rib or wrist region), tunnel it through
the walls, and splice it directly to the bedroom wiring, circumventing
the damaged section of master cable.
If the redirected wire isn’t long enough to reach
the bedroom, you splice an intervening piece of wire (i.e., the sural
nerve) cut out from a part of the basement you rarely use. In order not
to lose television function, you simply insert the TV plug into another
living room outlet (i.e., establish alternate connections). Although
this procedure may not be as desirable as replacing the master cable,
you, nevertheless, now have power in the back bedroom.
Case Studies:
I observed Zhang carry out peripheral
nerve-rerouting operations in three individuals with SCI. In addition, I
have interacted with two former patients.
Case #1:
Last year, 31-year old Yang acquired a T9-10 injury after falling
at work. The surgery’s
primary goal was to restore some of Yang’s lower extremity function,
especially bladder control. Yang’s 3-4-hour surgery was the most
involved of the three operations I observed.
Initially, Zhang detached for later use a sural
nerve segment from Yang’s calf. He
then proceeded to isolate an intercostal nerve from Yang’s rib region,
maintaining the nerve’s connection to the spinal cord. Next, Zhang
exposed Yang’s sacral nerve roots that control urogenital muscles.
After he sutured the detached sural nerve segment to the intercostal
nerve to make it long enough to reach this sacral region, the combined
intercostal-sural nerve was connected to the sacral nerve roots.
Yang demonstrated some restored sensation in body areas
controlled by the recipient sacral nerves (see dermatome chart) hours
after surgery (This quick initial recovery is due to decompression).
Case 2:
Although 31-year old Wang had retained some hip function after
his lumbar injury, he had lost bladder control. In this case, a nerve
that led to Wang’s functional hip was connected to a nearby
dysfunctional nerve that served the urinary system. Specifically, the
gluteus inferior nerve (originating from the L-5, S-1,2 spinal-cord
level) that innervates the gluteus maximus muscle was connected to the
injury-affected pudendal nerve (originating from the S-2,3,4 spinal-cord
level) that serves the urogenital muscles. Because of the nerves’
physical proximity, no intervening graft was needed. Overall, this was a
much less complicated operation, requiring only an hour to complete.
Case 3: Although
involving a peripheral nerve SCI treatment, the third surgery
represented a fundamentally different procedure, which Zhang has
performed in more than 12 patients, and is included because of its
radical nature.
This case involved
36-year old Chu, who had recently become a C-4 quadriplegic due to a
construction accident. In Chu’s operation, detached, sural nerve
segments were inserted directly into his injured spinal cord. These
segments were initially scraped to expose nerve fibers and, after scar
tissue was removed from and incisions made in the remaining cord,
inserted lengthwise without suturing. The next day, Chu, who had
previously possessed only residual bicep function, was able to move his
hands.
Follow-Up Case 1: Huocheng
acquired a T11-12 injury in a 1997 motorcycle accident when he was 25.
The following year, Zhang rerouted an intercostal nerve from one side of
Huocheng’s body to the lumbar nerve roots and, in turn, an intercostal
nerve from the opposite side of his body to the sacral nerve roots.
These two nerve reroutings together restored much of
Case 1: Huocheng
acquired a T11-12 injury in a 1997 motorcycle accident when he was 25.
The following year, Zhang rerouted an intercostal nerve from one side of
Huocheng’s body to the lumbar nerve roots and, in turn, an intercostal
nerve from the opposite side of his body to the sacral nerve roots.
These two nerve reroutings together restored much of 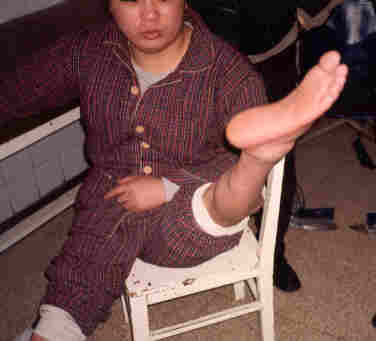 Huocheng’s
lower extremity function. For example, he now has considerable upper-leg
muscle control and
sensation down to his feet. Huocheng can now walk with crutches without
leg braces and has greatly improved bowel and bladder control.
Huocheng’s
lower extremity function. For example, he now has considerable upper-leg
muscle control and
sensation down to his feet. Huocheng can now walk with crutches without
leg braces and has greatly improved bowel and bladder control.
Follow-Up Case 2: In 1989, Bido became
injured in the lumbar region at age 17 after a car accident in Iceland.
After rehabilitation, she was able to walk using hip muscles in
conjunction with stiff braces that extended to her waist. Bido is the
daughter of Audur Gudjonsdottir, who was recently honored as Iceland’s
“Woman of the Year” for ongoing SCI advocacy efforts, including
spearheading the aforementioned WHO conference.
 After
a facilitating request from Iceland’s President Vigdis Finnbogadottir,
Zhang traveled to Iceland in 1995 to surgically repair and remove scar
tissue from Bido’s spinal area. Audur, a nurse, indicated that so much
scar tissue was removed that “both of my hands were full of it.”
That operation alone restored some function. Audur believes that “each
individual who sustains SCI should have an operation like that some time
after the accident.” She adds: “as expected, the body attempts to
heal itself with scar tissue, which is a band aid. When the band aid is
removed and the pressure alleviated from the spinal cord or the nerve
roots, things begin to work again.”
After
a facilitating request from Iceland’s President Vigdis Finnbogadottir,
Zhang traveled to Iceland in 1995 to surgically repair and remove scar
tissue from Bido’s spinal area. Audur, a nurse, indicated that so much
scar tissue was removed that “both of my hands were full of it.”
That operation alone restored some function. Audur believes that “each
individual who sustains SCI should have an operation like that some time
after the accident.” She adds: “as expected, the body attempts to
heal itself with scar tissue, which is a band aid. When the band aid is
removed and the pressure alleviated from the spinal cord or the nerve
roots, things begin to work again.”
In 1996, Zhang returned to Iceland to reroute
Bido’s intercostal nerve to her lumbar nerve roots. As a result of
these surgeries, Bido’s ambulatory ability has greatly improved even
though the surgeries occurred many years after injury. According to
Audur, “Bido has motor function in both legs down to the ankles. As
such, she is now able to walk using braces that end below the knees. She
bends both knees during walking, and her balance is much better.”
Conclusion:
Increasingly, it seems that the most exciting SCI
therapeutic breakthroughs are originating in numerous places other than
America. Although American neuroscience is unrivaled, for a variety of
reasons - the pros and cons of which can be debated extensively - it has
been difficult to translate this scientific excellence into real-world
SCI therapies. Even when the initial scientific breakthrough happens in
America, the bench-to-bedside transfer of knowledge that transforms this
breakthrough into useful therapies often seems to occur elsewhere.
One potential reason has been implied by
Christopher Reeve, the well-known actor with SCI whose foundation
greatly contributes to and influences the nature of SCI research in this
country. Commenting on a peripheral nerve-routing operation carried by
Italy’s Brunelli, Reeve has stated “I think it is pretty immoral
because you have to follow a sequence. You’ve got to go from rats, a
lot of rats. Then you have to go to bigger animals, pigs hopefully, not
monkeys. You’ve got to demonstrate safety and efficacy.” (see
http://care cureatinfopop.com).
Reeve’s opinion reflects the prevailing
conservative approach of the American SCI research community, which
believes that serving its needs for scientific rigor is the best way to
serve the needs of people with SCI for new therapeutic options. However,
as someone who was extensively involved in setting SCI research
priorities in this community, I believe that the cows will come home a
long, long time before the pigs tell us anything truly useful.
Dr. Zhang’s peripheral-nerve-rerouting approaches
appear extraordinarily promising for restoring significant function
after SCI. In the spirit of
cooperation, we need to open-mindedly develop synergistic, mutually
beneficial collaborations that can evaluate innovative procedures such
as his and, more importantly, facilitate new understandings. One of
Zhang’s foremost desires is to see a professional exchange in which
his colleagues and their American counterparts would be able to visit
and learn from each other’s experience.
Society’s continued evolution into a “global
village” has allowed us to share technology so we can order a
comparable McDonalds Big Mac hamburger regardless of whether we are in
China or America. Given that we can share such culinary technology, it
would be an absurd sense of priorities not to be able to somehow share
SCI therapeutic knowledge that would benefit so many.
If we can bring together all the exciting SCI
developments throughout the world, restoration of function would no
longer be some distant pie-in-the-sky dream but a real-world expectation
now. It’s time to pull it all together. No more excuses. Let’s roll.
Acknowledgements & Resources: Special
thanks are extended to Dr. Shaocheng Zhang, his colleagues, and
superiors for extensive hospitality. Dr. Zhang can be reached by mail at
32-43-301, Zhongyuan Rd., Shanghai 200433, China or by fax at
001-86(country code)-21(city code)- 65346003.
For more-technical summaries
of Dr.
Zhang’s peripheral nerve rerouting procedures, click here.
For those who are potentially interested in this
peripheral nerve rerouting surgery, Zhang is willing to consider foreign
patients, who would stay in a modern foreign-guest clinic or is willing
to travel to America to carry out the surgery if an appropriate
collaborative relationship can be established with an U.S. hospital.
Adapted from article appearing in Paraplegia News, April, 2002 (For subscriptions, contact www.pn-magazine.com).