
Although
much of my professional career has involved large, institutionally
funded research programs, I have been consistently amazed by how often
the individual can make a difference. For example, Audur Gudjonsdottir
(with author in photo), an Icelandic nurse, had little experience with
spinal cord injury (SCI) until her daughter got severely injured twelve
years ago in a car accident. With a committed mother’s relentless
energy, Gudjonsdottir started searching the world for therapies that
could help her daughter.
One indirect outcome of her search was a recent
conference held in Rey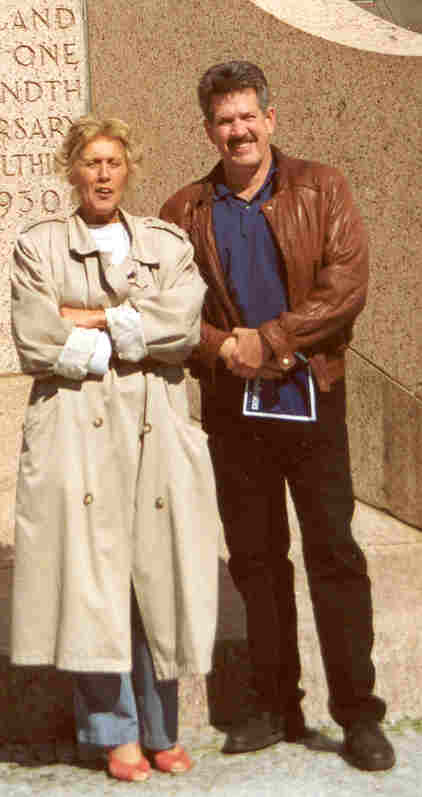 kjavik, Iceland on June 1-2, 2001. The conference,
“New and Emerging Approaches to SCI,” was sponsored by the World
Health Organization (WHO) and Iceland health officials.
kjavik, Iceland on June 1-2, 2001. The conference,
“New and Emerging Approaches to SCI,” was sponsored by the World
Health Organization (WHO) and Iceland health officials.
The Icelandic setting influenced the meeting in
many subtle ways. First, as the Vikings bridged the new and old worlds a
thousand years ago through Iceland, the country seemed to be an ideal
location to integrate divergent world SCI perspectives.
Due to the convergence of tectonic plates, part of Iceland
geologically resides in North America and part in Europe. The fact that
the conference reflected neither an American nor European dominated
endeavor helped to create a more neutral setting that was unencumbered
by any over-riding SCI ideology.
Second, because Iceland is a sparsely populated
country with relatively few SCI cases, it must reach out to other
countries to supplement its expertise. As a result, Gudjonsdottir could
not merely rely on the local experts but had to search abroad for SCI
therapeutic options. The
more expansive, international perspective she acquired clearly molded
the conference by open-mindedly ensuring that diverse SCI approaches
were included, ranging, for example, from mainstream to alternative
medicine, from the status quo to the controversial, from the large
academic medical center to the small independent clinic, and from
Western to Eastern medicine. The goal was to be inclusive not exclusive.
Third, many of Iceland’s leaders united behind
Gudjonsdottir’s
 efforts.
For example, the country’s popular, Ex-President Vigdis Finnbogadottir
(front row center in thumbnail photo) became an additional force behind
the conference. In another example, Lara Margaret Ragnarsdottir (sitting
to the left of President Vigdis), Iceland parliament member,
participated in the conference’s strategic discussions with the goal
of developing an SCI focus at the Council of Europe. In a third example,
the Mayor of Reykjavik hosted a reception attended by the ambassadors of
participating countries. The reception was held in one of Iceland’s
most famous buildings, the Hofdi, the site of the 1986 Reagan-Gorbachev
summit.
efforts.
For example, the country’s popular, Ex-President Vigdis Finnbogadottir
(front row center in thumbnail photo) became an additional force behind
the conference. In another example, Lara Margaret Ragnarsdottir (sitting
to the left of President Vigdis), Iceland parliament member,
participated in the conference’s strategic discussions with the goal
of developing an SCI focus at the Council of Europe. In a third example,
the Mayor of Reykjavik hosted a reception attended by the ambassadors of
participating countries. The reception was held in one of Iceland’s
most famous buildings, the Hofdi, the site of the 1986 Reagan-Gorbachev
summit.
Fourth, augmented by the energy of continuous,
Arctic Circle summer daylight, Icelandic hospitality generated an
incredible esprit de corps, enthusiasm, and commitment to move the field
forward.
Finally, although many men contributed to this
conference on a predominately male disorder, Icelandic women were the
strategic energy behind all levels of the meeting, ranging from
Gudjonsdottir’s injured daughter to Iceland’s former president.
Perhaps, this unique conference, which brought in an infusion of fresh
ideas, reflected a more feminine viewpoint on cooperation and, in turn,
problem solving.
Finnbogadottir opened the meeting with a discussion
of SCI as a human rights issue. She emphasized that medical research is
one mechanism by which people with SCI can be meaningfully integrated
into society and enjoy mankind’s most fundamental freedom of
self-determination. Finnbogadottir noted that the overall goal of
today’s exciting SCI research “should not be viewed as making one
whole again because the spirit is always whole. The goal is empowerment,
freedom of self-determination, and the ability to manifest the spirit
within.”
About 30 scientists attended the conference,
including representatives from Brazil, China, England, France, Iceland,
Israel, Mexico, Russia, Sweden, and the United States.
Summaries:
Precursor
Cell Transplantation: Paul Reier summarized his recently completed
clinical trial in which human embryonic spinal cord tissue was
transplanted into humans with post-traumatic progressive syringomyelia.
The study showed that the procedure is safe, feasible and obliterates
the cyst. Reier now believes that fetal tissue research is essentially
stem cell research.
Reier has also evaluated whether cellular grafting
can augment spontaneous repair processes by investigating the plasticity
of respiratory function following cervical injuries in rats. He has
found that a unilateral lesion can induce changes in respiratory
function at both segmental and suprasegmental levels, including upstream
effects in a brainstem respiratory generator. In animals with C2
hemisection, fetal grafts favorably influenced several of these
compensatory changes.
Reier is exploring alternatives to fetal-derived
CNS stem or precursor cells, including the potential of certain cancer
cells to transform themselves into neuronal like cells. Specifically, he
has shown that grafts of purified and retinoic acid-treated human Ntera2
neurons into chronic C4-5 contusion lesions (i.e., six-month
delayed grafts) can differentiate into neuronal subtypes and survive for
a year post-transplantation without tumor formation.
Second, Evan Snyder discussed how neural stem-cell
biology might play a therapeutic role in SCI. His research, primarily
using a rat model of a contused cord focused on motor neurons, shows
that stem cells can not only differentiate into neurons that integrate
into circuitry, but also give rise to the cells necessary to support
them. He believes that there is much communication amongst stem cells
and between stem cells and the damaged host. For example, stem-cell
differentiation is triggered by repair signals issued by the damaged
spinal cord host. His overall goal is to try to understand the various
molecular signals and then to try to harness and exploit them to enhance
more effective recovery after SCI.
Third, Semion Rochkind discussed the use of
low-power laser treatment to enhance the regeneration and repair of a
reconstructed injured spinal cord. Specifically, the spinal cords of 31
adult rats were transected. Rat embryonic spinal cord cells were
cultured, adhering to microcarriers (MCs) and forming cell-MCs
aggregates. After these aggregates reached intensive sprouting, they
were implanted into the transected spinal cord of 24 rats. The implants
served as regenerative and repair sources for reconstructing neuronal
tissue. During 14 post-operative days, 780-nm laser treatment was
applied transcutaneously 30 minutes to the implanted spinal cord area of
15 of the 24 rats. The remaining rats underwent spinal cord transection
with no implantation or laser treatment. Somatosensory evoked potential,
histological, and immunohistochemical analyses were carried out. The
results indicated that the most effective re-establishment of limb
function and gait performance, transport of electrophysiological signals
and histological parameters (indicating growth of the implanted tissue
in the injured area) occurred after nerve cell implantation and laser
irradiation, compared to nerve cell implantation without laser
treatment.
Fourth,
Fernando Ramirez discussed his use of xenotransplants to treat 47
patients with SCI over the past decade. The program targets those who
have sustained a compression injury in which some neurons remain
structurally intact across the injury site.
Initially, his surgical team removes bone fragments and scarring
tissue from the injury site. Any cysts that have developed are drained,
and a shunt is inserted to keep fluid from accumulating.
The spinal column is then reconstructed and strengthened.
Following this surgery, blue shark embryonic neuronal cell
cultures are injected within the dura mater. This procedure is based on
xenotransplantation therapies developed by Swiss physician Dr. Paul
Niehans beginning in the 1930’s and, in turn, by German scientist Dr.
Wolfram Kuhnau. Ramirez stated that the transplanted cells would
eventually form an infrastructure matrix that will accommodate neural
transmissions, and, in turn, restore some function over time.
Peripheral
Nerves: Tarcisio Barros has grafted peripheral nerve tissue into the
spinal cord gap caused by gunshot wounds in seven male adults with
thoracic level injuries. The gap is repaired using a peripheral nerve
bridge obtained from the sural nerve plus fibroblast growth factor and
fibrin glue. The patients were evaluated according to the ASIA/IMSOP
standards, and with magnetic resonance imaging and somatosensory evoked
potential. After 30 months, the grafts remain viable. Although no change
has been observed in motor or sensory recovery, less spasticity was
observed in the operated group.
Second, Giorgio Brunelli has rerouted the ulnar
nerve to leg muscles. The nerve is cut at the Guyon canal and elevated
through a zigzag approach. Motor branches for adductor pollicis and
first interosseous, for interossei, and for flexor carpi ulnaris and
flexor digitorum profundis of the little and ring finger are
respectively sutured to the motor branches for gluteus medius and
maximus and for quadriceps (the latter by means of an intercalated sural
nerve graft). Temporarily, the patient has to think to move the hand to
obtain hip movement. Rudimentary walking is regained with the help of a
light walker. EMG shows interference of the muscle is under volitional
contraction. Proprioceptive sensation is also regained over time.
Third, Zhang Shaocheng has rerouted the intercostal
nerve to spinal cord nerve roots below the injury. Specifically, after
microsurgically releasing and decompressing the cord, intercostal nerves
were transferred and bridged to the root that controlled the function to
be restored (e.g., muscle function, bladder control, or sensation). Over
30 patients followed an average of 2.5 years regained lower extremity
muscular control and could stand up and walk a short distance with
crutches and braces. Many had improved bowel and bladder control and
proprioception recovery.
Avulsed
Nerve Roots: Thomas Carlstedt’s has replanted avulsed ventral
roots, frequently caused from motor vehicle accidents, into the cord.
These implanted roots serve as a conduit for outgrowing motor axons. The
procedure restores some useful function about 30% of the time and also
reduces the pain associated with this type of injury. The first signs of
recovery are often not observed until 9-12 months after surgery.
New
Supporting Circulatory and Physiological Connections: Harry
Goldsmith discussed the transposition to the injured cord of omentum, a
highly physiologically active, stem-cell-containing tissue that hangs
like an apron over the intestines and lower abdomen area. The omentum is
surgically tailored to create a pedicle of sufficient length with intact
blood and lymphatic circulation to reach the injury site. The omental
pedicle is tunneled underneath the skin, placed over the exposed cord,
and sutured to the dural membrane edges.
The procedure was used to treat a woman with a nearly totally
transected cord. In this case, the scar tissue that filled the 1.6-inch
gap in her cord was replaced with an omental-collagen bridge. Prior
research with animal models, discussed by another speaker. Jack de la
Torre, has shown that this procedure promotes regeneration and
adrenoreceptor contact distal to the transection.
The patient has gradually gained strength and control of muscles
below the injury, including leg movement. Her MRI now shows the
continued development of structure connecting the spinal cord segments.
Second, Hernando Rafael reviewed his experience
with grafting an unattached piece of omental tissue over the injured
cord and connected it to a surrounding vascular source.
Over 13 years, he has treated 232 patients with traumatic SCI
with the procedure. About 43 percent have neurologically improved,
including 43 who are walking with or without the use of orthopedic
devices.
Third, Georgie Stepanov has used reconstructive
microsurgical vascular operations to revascularize the injured cord by
displacing the intercostal neurovascular fascicle into the cerebrospinal
channel and also by microsurgical omentomyelopexy. The method of suture
of the vessels with small diameter allowed them to perform microsurgical
anastomosis of the Adamkevich’s artery. The procedure has been applied
to several patients with encouraging results.
SCI in the
Developing World: Based on his Red Cross experience treating the
Afghan war wounded in Pakistan and the Romanian poor, Anba Soopramanien
discussed SCI rehabilitation in the developing world. Most of the
world’s SCI patients do not have access to the sophisticated, costly,
rehabilitative technology that those in developed nations take for
granted. For example, Somalia’s $11 per capita health-care expenditure
(compared to about $1,800 in Iceland and $4,700 in the U.S.) can do
little to promote SCI rehabilitation. Given such economics, Soopramanien
felt, among other things, that Western-trained SCI professionals should
supplement their expertise with the wisdom offered by more affordable
and accessible traditional or indigenous medicine. Overall, there is
little appreciation of the concept of integrated SCI health care in
developing countries. To truly alleviate the world’s SCI-related
suffering and mortality, we must work with the third world as a partner
to develop new SCI-care approaches, strategies, and paradigms suitable
to unique cultural conditions.
Alternative
& Eastern Medicine: Laurance Johnston provided an overview of
various alternative, complementary, energy-based, or non-mainstream
therapies that have the potential to benefit individuals with SCI.
He believes that these therapies can not only can help a variety
of secondary conditions but have the ability in some people, for certain
injuries to restore function. Alternative therapies highlighted included
Traditional Chinese Medicine approaches (e.g., acupuncture and qigong),
Ayurvedic medicine, surgical interventions, craniosacral therapy,
chronologically controlled developmental therapy, homeopathy, and
electromagnetic approaches.
Johnston summarized the results of a self-report,
pilot study he carried out in 13 paralyzed veterans using a commercially
available Ayurvedic multi-herbal product (ReGenTM Maharishi
Ayurveda Products). The anecdotal results suggested that the product
exerted a variety of subtle effects in many subjects, e.g., reduced
spasticity. Others have shown that extract of mimosa pudica, a key
herbal component of the product, can promote regeneration in rat
peripheral nerve injuries.
Second, Margaret Naeser summarized several Chinese
studies that she had reviewed for a 1997 NIH Consensus Conference on
acupuncture. Although none had a control group, 94% of the 360 treated
patients regained some function, including reduction in muscle spasms,
increase sensation, and improved bowel and bladder function. The authors
recommended electroacupuncture along the bladder meridian (paravertabral)
area and beginning acupuncture as soon as possible after injury.
Additional studies published since 1997 supported these findings.
From her own work, Naeser noted that stimulating
acupuncture points with low-level lasers (5-500 mW, red beam or near
infrared, 600-1000 nm wavelength) reduces muscle spasticity in the hand
and foot and promotes decubitous ulcer healing. Evidence indicates that
the effects may be mediated through the increased production of cellular
adenosine tri-phosphate (ATP).
Third, Albert Bohbot discussed laserpuncture, a
therapy based on Traditional Chinese Medicine and a quantic explanation
of the energetic physiology of the acupunctural network. Laserpuncture
focuses on a new matrix of 300 acupuncture points located on the abdomen
and back. With the treatment, an infrared laser triggers a dialog with
the body under the lesion in the form of tingling, hot, cold sensations.
The propagated sensation along the meridians is qi expression.
The choice of acupuncture points is patient specific.
Laserpuncture has promoted motor, sensation, and visceral recovery.
Bohbot believes that with laser therapy, the brain is able to convert
the electrochemical nervous impulse conduction into an electromagnetic
post-lesion conduction, through the conversion of wavelength of the
potential of normal depolarization, allowing it to cross the lesion.
Acute
Injury: Jack de la Torre discussed the use of fructose
1,6-diphosphate combined with dimethyl sulfoxide to treat acute spinal
cord trauma. Extensive research shows the benefit of dimethyl sulfoxide
in stabilizing spinal cord trauma and fructose diphosphate as a
high-energy substrate to the injured tissue. This cocktail therapy
addresses some of the immediate physiological, biochemical, and
metabolic problems associated with acute SCI, such as reduced spinal
cord blood flow, free radical formation, sodium channel activation,
inflammatory reaction and energy substrate depletion.
Second, Anders Holtz reviewed various neurosurgical
considerations following acute SCI. For example, before surgery, there
is a need to be aware of the secondary injury damage stemming from
residual compression; to establish the extent of neurological damage
using ASIA/IMSOP criteria; and to radiologically characterize the
injury. Initially, it is also important to focus on the respiratory
system, to help the cardiovascular system, and to initiate
methylprednisolone treatment within the drug’s therapeutic window.
Overall, the aim of surgery is to minimize neurological deterioration,
to restore alignment and stabilization, to facilitate early
mobilization, to reduce pain, to minimize hospital stay, and to prevent
secondary complications. Holtz summarized some of the factors that are
often used to choose surgical over conservative treatment. Specifically,
surgery is often preferred if there is concern with secondary injury,
the fractures are unstable, there is a contusion to the cord, there is
canal compromise, there is ongoing neurological deterioration, the
lesion is incomplete, it is a lower injury, and the patient is younger.
Functional
Electrical Stimulation (FES) and Orthotic Devices: Jack Edwards
reviewed his upright mobility programs, which have cumulatively treated
470 people with SCI. With training, most users of reciprocal gait
orthoses (RGO) can walk distances of over 300 meters at speeds from 0.2
to 0.5 m/s. Furthermore, after standing rest, they can continue up to
distances of 0.6 Km without sitting down. The most common complaint was
upper limb pain and discomfort, especially the hands. To reduce these
effects, Edwards used a number of advanced orthotic designs, including
hybrid RGO–FES systems and microprocessor controlled orthotic knee
joints, which allow the RGO knee to bend during the swing phase of
walking. The devices reduced the force on the hands by 15% and energy
expenditure by up to 30%. Overall, the incidence of urinary tract and
lower respiratory tract infections, spasms, and pain were less in
individuals that were part of their upright mobility program compared to
general wheelchair users.
Second, Maurizio Ferrarin discussed how
biomechanics allows the optimal design of mechanical orthoses for
restored walking in paraplegics and provides information for the
development of musculoskeletal system models useful for the design and
test of strategies for the control of FES systems. Multi-factorial
movement analysis techniques allows the quantification of the functional
advantages of a single treatment, the comparison of different solutions,
and the adaptation of a device to the characteristics of a specific
individual. The following examples were presented: the development of a
new hip joint for the RGO that provides a more physiologic pelvic
rotation; the analysis of the improvements provided to patient
hemodynamics by the combination of FES to the RGO; and the development
of a control strategy for FES-induced standing up, based on the EMG
signal of supralesional muscles.
Third, Anatoly Vitzenson has used FES muscle stimulation to artificially
correct movements in 900 patients with SCI. In his study, which focused
on lumbar-sacral injuries, the hip and knee joints muscle extensors were
stimulated in 20 sessions. The program resulted in improved
anthropomorphous walking properties; enhanced walking velocity, cadence,
and step length; decreased fatigue; growth in muscle force and
electrical activity during maximal effort; and partial normalization of
innervative gait structure. Also, the therapy has restored some pelvic
organ function. Vitzenson believes that excellent, good, and
satisfactory results have been obtained in 6%, 83%, and 11% of his
patients, respectively.
Fourth, Michael Keith summarized the results of
implanting the FreehandTM neuroprosthesis to recreate
gripping hand motion in quadriplegics. To date, over 200 neuroprostheses
have been implanted using 50 surgical and 55 rehabilitation centers.
Typically, the implanted muscles are those that represent key movements,
such as the thumb abductors, flexors, extensors, and finger flexors and
extensors. The chosen muscles are strong and have good innervation. The
muscles after having been instrumented by the implantable device are
then programmed by an external computer. The patient carries a portable
device, which has information regarding the quality of muscles and the
patterns of motion that the patient is to have. Up to eight muscles can
be controlled by a variety of control sources. Patient independence was
improved by average of 85% over their pre-operative state. Adverse
effect incidence has been low.
Fifth, Nick Donaldson discussed possible locations
for and issues surrounding the placement of implanted stimulators.
Overall, he believes that implanted stimulators are more convenient to
use, give more repeatable responses, and more muscles may be stimulated.
However, there is no consensus about where the electrodes should be
sited. Possible sites include nerve twigs, nerve branches, nerve trunks,
nerve roots, or the spinal cord. The most promising methods seem to be
stimulation of the nerve roots in the cauda equina and spinal cord
microstimulation.
Finally, Antony Tromans summarized a variety of
potential FES applications beyond limb movement, including respiration;
bladder, bowel, and sexual function; and skin problems.
Aggressive
Physical Rehabilitation: As the likelihood of real-world SCI
therapies increases over time, Arnie Fonesca emphasized that it will be
important to have follow-up aggressive physical rehabilitation to
maximize function in long dormant muscles. Professional athletes
rehabilitate more efficiently because they have access to the best care
and equipment and are surrounded by highly motivated people to
complement their own skill and motivation. Fonesca believes that if we similarly treated SCI, functional
recovery would be much greater. At minimum, the individual would be in
better physical shape, better able to endure SCI secondary conditions,
and have a self-confidence boost. As an example, Fonesca discussed how
aggressive physical rehabilitation enhanced function following omental
transposition therapy.
Conclusion:
In conclusion, the conference’s
whole-is-greater-than-the-sum-of-the-parts philosophy believed that the
big breakthroughs will happen only if we open-mindedly bring together
divergent yet often synergistic treatment and research perspectives.
Recognizing that today’s cutting-edge, scientific insights are
often tomorrow’s anachronisms, this conference attempted to set aside
the illusion of knowledge that so frequently inhibits discovery.
Adapted from article appearing in Paraplegia News, September,
2001 (For subscriptions, contact www.pn-magazine.com.