
Over the past several decades, I have observed
remarkable progress in our understanding of spinal cord injury (SCI), a
disorder once considered so intractable that its repair was described as
the Holy Grail of neurological research. As demonstrated by innovative
therapies being developed throughout the world, this Grail is increasingly
within our grasp. So many promising procedures are in the developmental
pipeline, it is difficult to keep track of them all.
However, due to a variety of regulatory, scientific
and societal barriers – the pros and cons of which are debated extensively
in the SCI community - the majority of the most exciting developments are
happening outside the United States. Nevertheless, this obstacle does not
stop motivated Americans from traveling great distances to avail
themselves of these function-enhancing therapies.
Currently, one of the most talked about therapies
involves the transplantation of olfactory ensheathing cell (OECs). This
procedure is carried out by Dr. Hongyun Huang, professor
 and
chief neurosurgeon, Chaoyang Hospital, Beijing, China, who I met at the
Congress of Neurological Surgery (Denver) and the Rehabilitation Institute
of Michigan (RIM).
and
chief neurosurgeon, Chaoyang Hospital, Beijing, China, who I met at the
Congress of Neurological Surgery (Denver) and the Rehabilitation Institute
of Michigan (RIM).
Dr. Huang acquired much his OEC expertise in the US,
as he worked three years in the laboratories of Dr. Wise Young (currently
of Rutgers University), a leading expert on the transplantation of OECs
into SCI animal models. Taking this expertise back to China, where the
bench-to-bedside, technology-transfer barriers are less insurmountable,
Huang developed his human OEC-transplantation procedures.
Regenerative Olfactory Tissue:
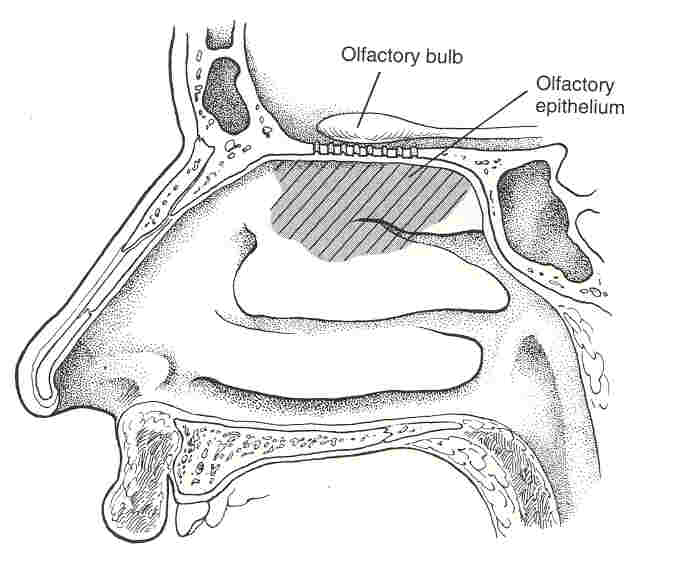
As discussed elsewhere,
the nose contains neurons that send signals to the brain when triggered by
odor molecules. The axons of these neurons are enveloped by OECs, a
special type of neuronal support cell that guides the axons and supports
their elongation. The bundles travel from the nose to the brain’s
olfactory bulb, where they make connections with other neurons. Because
olfactory tissue is exposed to the external environment (i.e., the air we
breathe), it contains cells with considerable regeneration potential,
including renewable neurons, progenitor stem cells, and OECs.
Through a relatively innocuous biopsy procedure,
olfactory tissue can be obtained from the nasal cavity. It can also be
retrieved from the olfactory bulb, but this requires an invasive
penetration of the cranial cavity that although unsuitable for human
patients has been the procedure for most of the supporting animal
research.
When transplanted into the injured spinal cord, OECs
theoretically promote axonal regeneration by producing insulating myelin
sheaths around growing and damaged axons, secreting growth factors, and
generating structural and matrix macromolecules that lay the tracks for
axonal elongation.
Different Approaches:
Keeping up with promising olfactory transplantation
procedures can be difficult because research teams use varying approaches.
For example, Portugal’s Dr. Carlos Lima
implants whole olfactory tissue obtained from the patient back into
his/her injury site. Lima believes that more than one cell type is needed
to maximize regeneration, including not only OECs but also olfactory
neurons and stem cells. To date, Lima has treated more than 20 patients.
In another example, an Australia team implants OECs,
isolated and cultured from the patient’s nasal tissue. Several patients
have been treated.
In contrast, Huang transplants OECs isolated not from
the patient but from fetal olfactory bulbs. Although fetal-tissue
transplantation is controversial in this country, American SCI scientists
also have used fetal tissue in promising research. As would be required at
any America institution, Huang’s hospital ethics committee approved his
clinical trials in advance. Huang has transplanted OECs into more than 300
patients with SCI, including several Americans, and thousands are on his
waiting list.
Immunological Acceptance:
In Portuguese and Australian procedures, no
immunological rejection of the transplanted tissue occurs because it is
patient derived; with Huang’s procedure, fetal-tissue’s undifferentiated
nature minimizes immunological rejection.
Procedure:
The following summarizes results recently published
in the Chinese Medical Journal (Chin Med J 2003; 116(10)).
Decompression: To ensure that improvement was
not merely due to surgery-associated decompression, patient MRIs had to
indicate the absence of compression before surgery. In addition, the cord
must have some structural continuity through the injury site, the
situation for most individuals with SCI.
Patient Demographics: Huang’s study included
139 men and 32 women, of which 114 were quadriplegics and 57 paraplegics.
Ages ranged from 2 to 64 (average 35) years, and the interval between
injury and admission varied from 6 months to18 years.
Cell Transplantation: Olfactory-bulb OECs are
grown in culture media for several weeks before transplantation. After the
spinal cord has been exposed through a limited laminectomy, 500,000 cells
are injected above and below the injury site. These cells presumably
migrate to the injury site. Animal studies suggest that the OECs survive
better when they are not directly injected into the injury site.
Functional Assessment: Function was assessed
before and 2-8 weeks after surgery using the “gold standard” ASIA
(American Spinal Injury Association) impairment scales, which include
motor-function, light-touch, and pin-prick scores.
Results: Improvement was noted for each of
these scores in five age categories (<20, 21-30, 31- 40, 41- 50, and >50).
Interestingly, even though it is often assumed that regenerative potential
is better in the young, pin-prick improvement was greatest for the 50+
category.
Possible Mechanisms:
Patients are often regaining some sensory and motor
function soon after surgery. The study design specifically eliminated
spinal-cord decompression as a possible cause for this rapid functional
improvement. Improvement is also too fast to be caused by neuronal
regeneration or axonal remyelination.
Huang speculates that OECs wakeup quiescent neurons
that still transverse the injury site, perhaps by altering the injury
site’s environment through secreting growth factors and producing adhesion
and matrix molecules.
Young notes that most neurons actually survive after
injury, but their axons have been disconnected. He hypothesizes that by
secreting a variety of growth factors, OECs may make the spinal cord more
plastic or adaptable; this, in turn, encourages local axons to shift their
connections.
American Patients:
To date, Huang has treated four Americans, including
Bob (photo, bottom right in front of hospital), who I met d uring
my visit to RIM. Bob, 46, sustained a C5 injury from diving into the
shallow water of Michigan’s Lake St. Clair on July 4, 1999.
uring
my visit to RIM. Bob, 46, sustained a C5 injury from diving into the
shallow water of Michigan’s Lake St. Clair on July 4, 1999.
Bob’s improvement came quickly, including wiggling
his toes hours after surgery. Three weeks after returning home, he
reported a variety of additional motor and sensory improvements. For
example, bowel and bladder function had improved. Specifically, Bob needs
to empty his bladder less frequently because it empties more fully.
Due to improved trunk control, Bob notes that he is
now able to “sit on the side of the bed for at least an hour going from
side to side with little effort and shift from lying back on elbows to a
sitting position by turning to either side and getting up.”
Bob’s triceps grew stronger, and his fingers gained
better control. “Everything is much easier to grab,” he says. “I used a
pair of scissors today cutting a wrapper off a Twizzler.” He scratches
with his fingers instead of his thumbs. “I can even reach behind my head
and neck to scratch my scar itch.”
Three months after surgery, Bob reports continued
improvement, especially in his hands. He also notes “my upper first then
lower abs have recently made an appearance.”
Conclusion:
Although the procedure has restored significant
quality-of-life-enhancing function in most patients, Huang emphasizes that
OEC-transplantation is not a “cure,” and patients must keep realistic
expectations. Before definitive conclusions are made, more long-term
patient follow-up is needed. In addition to promising SCI results, a
limited number of cases suggest that OEC transplantation may provide
benefit to patients with multiple sclerosis, ALS (i.e., Lou Gehrig’s
disease), and stroke.
A growing number of SCI scientists, including myself,
who have visited China, believe this country will play a major role in the
development of future SCI therapies. In China, thousands with SCI have
been treated with a variety of function-restoring surgeries, none of which
are currently performed in the US.
If Americans with SCI are to benefit from China’s
ever-growing clinical experience, we need to proactively and open-mindedly
develop bridge-building, knowledge-disseminating collaborations,
including, for example, cooperative clinical trials.
Adapted from article appearing in Paraplegia News,
April, 2004 (For subscriptions, contact www.pn-magazine.com).