Experts have endorsed chiropractic as one of the most
effective ways of treating such pain, discouraging traditional approaches
of bed rest, medication, and surgery as counter productive. Most notably,
a 1997 U.S. Agency for Health Care Policy (AHCP) report stated,
“Chiropractic is now recognized as the principal source of one of the few
treatments recommended by national evidence-based guidelines for the
treatment of low-back pain, spinal manipulation.”
With 35-million Americans visiting 60,000
chiropractors each year, chiropractic is the nation’s third-largest
healthcare profession after medicine and dentistry. Of these people, 70%
use chiropractic for back pain; 25% for head, neck and extremity pain; and
5% for other disorders.
Due to its popularity, including among individuals
with physical disabilities, chiropractic should no longer be considered
“alternative medicine” but a key component of our healthcare system that
synergistically complements - not opposes - conventional medicine.
Chiropractic can help not only caregivers, who put
their backs in harm’s way, but, as discussed below, also enhance the
wellness of some people with spinal cord dysfunction and other
disabilities, whose wheelchair living (e.g., transfers, bad posture,
imbalanced muscle development, etc) aggravates physical problems amenable
to chiropractic treatment.
Definition:
Chiropractic focuses on diagnosing and treating
musculoskeletal disorders that affect the nervous system and, as a
consequence, general health. More specifically, the Association of
Chiropractic Colleges defines chiropractic as “A healthcare
discipline that emphasizes the inherent recuperative power of the body to
heal itself without the use of drugs or surgery. The practice of
chiropractic focuses on the relationship between structure (primarily
spine) and function (as coordinated by the nervous system) and how that
relationship affects the preservation and restoration of health. In
addition, doctors of chiropractic recognize the value and responsibility
of working in cooperation with other healthcare practitioners when in the
best interest of the patients.”
Chiropractic’s core philosophy differs from
conventional medicine, which believes we are the sum of our body parts
(e.g., organs, cells, or molecules); if we fix the parts, the body will be
repaired. In contrast, chiropractic grew out of a holistic vitalism
philosophy, which says that the body has an innate life force (e.g., like
qi or prana in Eastern-healing traditions) that flows down from the brain
with the nervous system and out from the spine to the periphery. Like
fixing a garden-hose kink, chiropractic adjusts musculoskeletal
distortions that inhibit this flow and, by so doing, enhances wellness.
History:
Chiropractic procedures have been a part of mankind’s
healing armamentarium since time immemorial, including use by ancient
Chinese, Egyptian, and Greek civilizations. Both Hippocrates (460-377
B.C.) and the influential Roman physician Galen (A.D. 129-199) recommended
vertebral adjustments to relieve ailments.
The f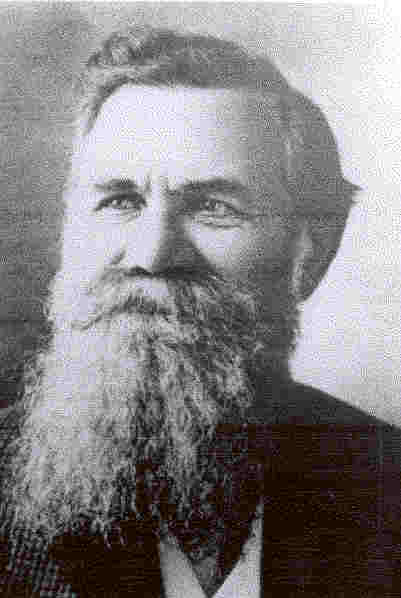 ounder
of today’s chiropractic was Daniel David Palmer (1845 –1913), a
self-educated man in medicine and science who practiced in Davenport,
Iowa. In 1895, through vertebral manipulation, he restored the hearing of
his building’s janitor, who had been deaf since a back accident 17 years
earlier. This incident gave birth to chiropractic, the term coined from
the Greek words praxis and cheir, meaning treatment by hand.
ounder
of today’s chiropractic was Daniel David Palmer (1845 –1913), a
self-educated man in medicine and science who practiced in Davenport,
Iowa. In 1895, through vertebral manipulation, he restored the hearing of
his building’s janitor, who had been deaf since a back accident 17 years
earlier. This incident gave birth to chiropractic, the term coined from
the Greek words praxis and cheir, meaning treatment by hand.
Much of the credit for chiropractic’s growth was due
to the organizational leadership of Palmer’s son Bartlett Joshua
(1881–1961), who at age 21 took over and built up the now well-known
Palmer School of Chiropractic in Davenport.
 He
was an innovator, who, for example, integrated nascent x-ray technology
into the profession, and was an effective chiropractic promoter and
defender. He cultivated and lobbied national figures and U.S. presidents,
and even employed future President Ronald Reagan as a broadcaster at his
World of Chiropractic (WOC) radio station.
He
was an innovator, who, for example, integrated nascent x-ray technology
into the profession, and was an effective chiropractic promoter and
defender. He cultivated and lobbied national figures and U.S. presidents,
and even employed future President Ronald Reagan as a broadcaster at his
World of Chiropractic (WOC) radio station.
Gradually, states approved chiropractic; Minnesota
was the first (1905), and Louisiana the last (1974).
Chiropractic faced vociferous opposition from
organized medicine, which essentially viewed it as a threat to its
healthcare monopoly. Because medicine did not include a
spinal-manipulation focus - preferring its pharmaceutical and surgical
approaches - it minimized the benefits that could accrue from this focus
emphasized by a competing discipline.
In defense of organized medicine, which had made huge
healthcare advancements as it transitioned into the 20th
century and cleaned up its own house by imposing rigorous professional
standards, many of the early chiropractic profession’s actions,
infighting, lax standards fueled criticism. Chiropractic emergence was
also handicapped, however, because it did not advocate drugs, and, as
such, could not cultivate strong financial, pharmaceutical-industry
allies. (e.g., on average, every U.S. physician receives >$14,000 each
year from the pharmaceutical industry’s marketing and promotional
campaigns.)
Organized medicine was forced to back down when a
landmark, 1987 federal anti-trust ruling found the American Medical
Association (AMA) guilty of a prolonged and systematic attempt to
completely undermine the chiropractic profession, often using highly
dishonest methods. By stopping the major source of organized resistance,
this case ushered in a new era of cooperation between physicians and
chiropractors.
In recent decades, Federal actions have increasingly
supported chiropractic, including: the 1974 authorization to the Council
of Chiropractic Education to accredit schools, the aforementioned AHCP
endorsement of chiropractic to treat lower back pain, the 1996 decision by
the National Institutes of Health to fund chiropractic research, and
President Clinton’s 2000 mandate that chiropractic be made available to
all active-duty military personnel.
Education:
Facilitating its current acceptance, the chiropractic
profession has adopted strict educational standards, comparable in rigor
but different in focus from medical education. Although both professions’
basic-science components are equivalent in study time, chiropractic
emphasizes musculoskeletal and neuroanatomical systems over medicine’s
pharmacological and surgical priorities. Furthermore, in contrast to
medicine’s broad clinical preparation, chiropractic clinical training is
specialized, focusing on the profession’s unique diagnostic and treatment
methods, which can only be mastered through extensive, hands-on practice.
Procedures:
Chiropractors focus on correcting disordered
vertebral joints, which include vertebrae and their boney projections
(called facet joints and spinous or transverse process es),
shock-absorbing cartilage discs, muscles, ligaments, and nervous tissue. Subluxations
- abnormalities of this vertebral complex - affect health by impinging on
nerve roots as they exit the complex through channels called
intervertebral foramen.
es),
shock-absorbing cartilage discs, muscles, ligaments, and nervous tissue. Subluxations
- abnormalities of this vertebral complex - affect health by impinging on
nerve roots as they exit the complex through channels called
intervertebral foramen.
Because of the complex’s inherent intricacy,
subluxations can result from numerous, interacting factors that upset the
complex’s homeostatic equilibrium, e.g., from unbalanced muscle tension
that pulls a vertebra out of alignment with neighbors. In turn, a specific
subluxation can create a chain reaction affecting other parts of the
spinal column. For example, neck pain may be the secondary consequence of
a pelvic misalignment.
Chiropractic emphasizes non-invasive therapies, such
as manual treatments, physical therapy, exercise programs, nutritional
advice, orthotics, and lifestyle modification.
The most common procedure is the spinal adjustment,
accomplished through diverse techniques. For example, with spinal
manipulation, using the vertebral projections as levers, a carefully
measured force is rapidly applied to the joint that carries it past its
voluntary range of motion but still well within the range permitted by
nature. The commonly heard “crack” is actually a vacuum-created, nitrogen
bubble bursting within the joint. In contrast, with spinal mobilization
procedures, the joint remains within its passive range of movement.
Depending upon the problem’s acute or chronic nature,
often multiple treatment sessions are needed, 6-10 being the average.
Studies show that the chiropractic risks are minimal.
For example, a 1996 RAND Corporation study concluded that 1.5 serious
complications occur from every million cervical manipulations. For
comparison sake, there are 1,000 serious complications per million from
taking over-the-counter painkillers.
Chiropractic & Physical Disabilities:
People with disabilities frequently use chiropractic.
For example, a Kessler Institute (N.J.) study indicated 23% of people with
SCI with chronic pain had used chiropractic (Nayak et al, J. Spinal
Cord Medicine, Spring, 2001).
Dr. Julet Hutchens, a chiropractor
(photo) who practices with medical doctors
and physical therapists, discusses potential SCD benefits:
“I have treated patients with spinal cord dysfunction
for four years, the first of which was my husband Eddy, a wheelchair
athlete and Mountain States PVA associate member. When I met him, he had
been paralyzed 16 years due to an automobile accident, in which he
sustained a complete T-10 spinal-cord transection.
I adjust Eddy usually 1-2 times per month depending
on his activity and discomfort level. I keep the majority of my
adjustments to him and other paralyzed patients above the injury level.
However, occasionally, I will perform more passive types of mobilization
to the pelvis, low back, and lower extremities. Eddy says the adjustments
give him instant relief to shoulder problems, upper/mid-back and rib pain,
and neck pain. A Denver Rolling Nuggets basketball player, he recommends
chiropractic treatments to his teammates to ensure their continued full
range of movement above and below the injury site.
I often treat shoulder and rib-related injuries in individuals with
paralysis that result from their excessive shoulder and arm use associated
with frequent wheelchair transfers. Often, a repetitive-use injury occurs,
which, if not taken care of, can lead to more severe shoulder problems,
even requiring surgery. Chiropractic treats the shoulders and ribs, giving
the patient relief. And with any repetitive-use injury, strengthening
exercises reinforce adjustments, preventing future injuries.
As with any person sitting for long time periods, posture becomes an issue
in wheelchair users. Most end up with neck and upper-back pain due to bad
posture. When we sit for a long time, we tend to slump forward, placing
extra stress on the neck and upper back. When I observe wheelchair
athletes, I see them leaning forward, resting their arms on their legs, or
leaning slightly forward and to the side, resting on a wheel. Such posture
places extra stress on the neck and upper back, and, as a result, the
muscles around the spine become weak and those in the chest become
tighter. These changes cause an imbalance between front and back muscles,
which can lead to pain. I work with the patient to rebuild muscle balance,
and restore motion in the spine that is restricted from such imbalance.
Teaching patients the difference between good and bad posture is
especially important so that they become aware of the small changes they
can make to alleviate some of their neck and back issues.
Active individuals with paralysis will develop a strong upper body to
compensate for their inability to balance themselves through the use of
abdominal, leg, and lower-back muscles as an able-bodied person would.
Because of this upper-body reliance, we want to keep it in good working
order, which is accomplished through a strong chiropractic and stretching
and strengthening programs. Shoulder or neck pain can impair one’s ability
to not only transfer in or out of a wheelchair but also to push it,
limiting overall mobility.
Adjustments, muscle work, and exercises keep the spine, shoulders, ribs,
and shoulder blades moving as they should in a painless, full range of
motion. These methods keep the joints lubricated, discs between the
vertebrae from deteriorating, and muscles and ligaments strong and
balanced. At the same time, it loosens muscles.
Overall, because they will be healthier, feel better,
and have more energy, all wheelchair users should receive regular
bodywork.
When I treat patients with SCI, arthritis that causes joint fusing,
post-polio, or cerebral palsy, I adapt my treatment to accommodate the
patient. Depending on their disability, I treat patients in their
wheelchair, or if comfortable, I will help them transfer to a treatment
table.
I try to choose the optimal treatment for the
specific patient, some of which are more passive or aggressive than
others. I also x-ray all patients with SCI to see exactly what is going on
in their spine, shoulders, etc. With SCI, the body compensates in one
area for the lack of motion in another. Because such compensation can be
observed through x-rays, the patient can be more effectively treated.”
Chiropractic Restoration of Function?
Dr. Dudley Delany, a chiropractor, relates an
anecdotal case suggesting that chiropractic therapy may have the potential
to restore some function after SCI. Specifically, when Delany was a
freshman chiropractic student, the school's president indicated that he
had became a paraplegic after a football injury but was able to regain
full recovery through chiropractic spinal manipulations. For further specifics,
see
http://www.webspawner.com/users/chiroscitx/index.html
Conclusion:
Most healing traditions have something valuable to
offer yet, at the same time, have limitations in scope. Allopathic
medicine emphasizes valuable pharmaceutical and surgical interventions,
chiropractic focuses on musculoskeletal system mechanisms that medicine
has ignored, and other traditions stress different therapeutic concepts
and modalities that also have great validity. It is as if medicine looks
at the world through red-tinted lenses, chiropractic blue lenses, and
other disciplines green or other colored lenses.
Unless we work together more in unity than
opposition, each discipline’s vision will remain inherently limited to the
detriment of all. However, if we open-mindedly accommodate divergent views
of what is possible, we create an expanded healing spectrum that will
benefit all, including those with spinal cord dysfunction.
Contact: Dr. Julet Hutchens, CLINIX, 7030 S.
Yosemite, Centennial, CO 80116 (303-721-9984).
Adapted from a two-part article appearing in Paraplegia News,
October & November, 2003 (For subscriptions, contact www.pn-magazine.com).
TOP