
Brian
Sternberg was not just a superb athlete; he was the best. In 1963, the
University of Washington junior established a world pole vault record of
16’8” and seemed destined to be the first to break 20 feet. His
gymnastic background had made him a strong, agile athlete, hence,
especially well suited for the new, flexible, state-of-the-art
fiberglass poles.
Practicing on the trampoline as he often did,
Sternberg tried a maneuver that he had routinely carried out in this
past. This time, something went wrong. Landing awkwardly on his neck, he
sustained a C4-5 spinal cord injury (SCI).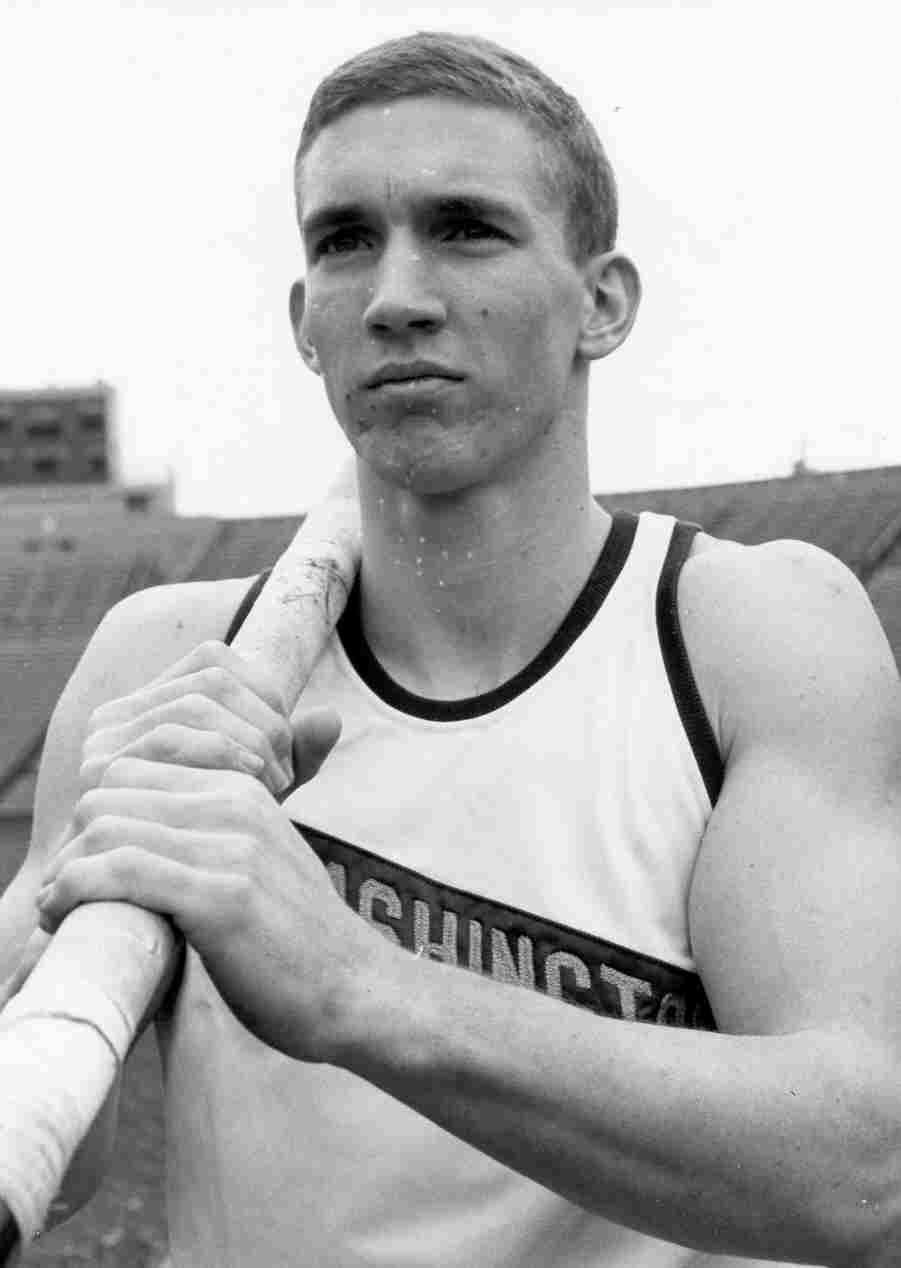
More than three decades later in 1996, surgeon
Harry Goldsmith operated on Sternberg, who says the omentum surgery
greatly increased his quality of life. For example, because
Sternberg’s injury affected the nerves controlling respiration, he
could only speak in a whisper before surgery. Since then, his voiced has
increased by about 60%.
“I wouldn’t have been able to have this
conversation with you before the operation”
Sternberg told me. He says his overall health and strength has
greatly improved. For example, the operation has reduced the
incapacitating pain that he once had.
“Before
the surgery, on a scale of 1-10, my pain averaged 8-13, “ Sternberg
says. “Now it is 1-2.”
He has more feeling in extremities and improved
circulation. He can stay upright for long periods of time, a problem
before the surgery. In a Sports
Illustrated article (September 21, 1998), Brian has stated that the
operation “has made all the difference in the world.”
RESEARCH COMMUNITY SKEPTICAL:
Omental transposition is a controversial surgery
used to treat spinal cord injury (SCI). In this procedure, the omentum,
a physiologically dynamic, fatty membranous tissue surrounding the
intestinal and lower abdominal region, is surgically lengthened and
placed over the area of injury.
Goldsmith pioneered this procedure for various
central nervous system disorders, including SCI. Currently associated
with the University of Nevada’s School of Medicine (Reno), Goldsmith
has spent much of his career investigating omentum’s therapeutic
potential. His work has stimulated many others who have now treated
thousands of patients for spinal cord injury, and other neurological
disorders, such as stroke, cerebral palsy, Alzheimer’s disease, and
Parkinson’s disease.
The procedure’s acceptance has grown greatly in
other parts of the world, such as in China where more than 3,000 people
with spinal cord injury have had omental surgery. In the United States,
however, the conservative SCI research community has been reluctant to
evaluate omental therapy for a variety of reasons.
First, many researchers urge caution when
considering a new therapy like this that involves an inherently risky
surgery that tampers with the spinal cord.
Second, omental surgery’s radical nature falls outside of
prevailing SCI research perspectives and priorities. As such, in a
“see-it-when-I-believe-it” attitude, the SCI scientific community
tends to see the omental approach’s flaws that reinforces their
preconceptions rather than the evidence that would require them to
change their view.
Third, although many have had omental surgery, the
value of this clinical experience, especially when originating in other
countries, does not count much in the U.S. scientific court of judgement.
Scientists believe that the only evidence that really matters is that
generated by rigorously designed, controlled clinical trials, which have
not as yet been carried out for omental surgery.
Fourth, the therapy’s image was dealt a blow
after a mid-1990’s controversy in which an unauthorized, recruiting
agent was accused of over promoting omentum’s therapeutic benefits. As
controversy enveloped the procedure, combined with some supposedly,
negative research findings (see below), the momentum for the therapy
shifted to other countries.
Goldsmith continues to be a tireless omental
therapy advocate. Several benefactors have recently donated $2 million
dollars to establish the Omental Research Foundation to support his
efforts. He plans to use these funds to help defer the high patient cost
of the surgery and fund basic-research pilot studies.
THE OMENTUM:
 The
omentum is a highly vascular, fatty tissue approximately 14 inches in
length and 10 inches wide that hangs like an apron over the intestines
and lower abdomen area. Although the omentum has been viewed as an inert
tissue bereft of significant biological function, scientists are now
discovering that it is an intriguing, physiologically dynamic tissue
with a considerable body of research that supports its therapeutic
potential (e.g., see Agner et al, Neurological Research, January, 2001 and The Omentum Application to Brain and Spinal Cord, edited H.S.
Goldsmith, Forefront Publishing, 2000):
The
omentum is a highly vascular, fatty tissue approximately 14 inches in
length and 10 inches wide that hangs like an apron over the intestines
and lower abdomen area. Although the omentum has been viewed as an inert
tissue bereft of significant biological function, scientists are now
discovering that it is an intriguing, physiologically dynamic tissue
with a considerable body of research that supports its therapeutic
potential (e.g., see Agner et al, Neurological Research, January, 2001 and The Omentum Application to Brain and Spinal Cord, edited H.S.
Goldsmith, Forefront Publishing, 2000):
·
Blood supply: The omentum contains angiogenic
factors that stimulate the growth of new blood vessels into whatever
tissue it is surgically placed next to, including the brain and spinal
cord (see figure).
·
Lymphatic System: The omentum is rich in
lymphatic vessels and tissue that are critical in removing metabolic
waste and excess fluid, destroying toxic substances, and fighting
disease.
·
Immune System: Omental areas called “milky
spots” are capable of generating specialized immune cells that
facilitate healing. For example, some scientists believe that the
migration of omental immune cells, called macrophages, can help repair
injured spinal cords.
·
Edema Absorption: The omentum’s lymphatic
system has an enormous capacity to absorb edema fluid, including that
associated with spinal cord swelling.
·
Source of Biological Material: The omentum is a
rich source of biological material that enhance tissue growth,
including angiogenic factors, key neurotransmitters, nerve growth
factors, and agents involved in inflammatory and immune processes.
·
Stem Cells: Evidence suggests that omental tissue
contains stem cells - omnipotent master cells that can differentiate
into a variety of cell types. For example, Dr. Ignacio Garcia Gomez
(Madrid, Spain) and colleagues demonstrated the presence of stem cells
in the human omentum (Neurological Research, 27, December
2005). These cells were shown to synthesize key growth factors that
promote vascularization when transplanted.
THE SURGERY:
Omental surgery, a six-hour operation, initially
cuts into the abdominal cavity to access the omentum. The omentum is
then gently separated from the colon and the stomach in a way that
maintains blood and lymphatic circulation (see illustration). The omentum is then surgically tailored to create a pedicle – a
piece of connected tissue of sufficient length with intact circulation
to reach the spinal cord injury site, like a square handkerchief would
be cut to make a long necktie. The omental pedicle is then tunneled
underneath the skin, placed over the exposed cord, and sutured to the
cut edges of the dural membrane surrounding the cord.
The omentum is then surgically tailored to create a pedicle – a
piece of connected tissue of sufficient length with intact circulation
to reach the spinal cord injury site, like a square handkerchief would
be cut to make a long necktie. The omental pedicle is then tunneled
underneath the skin, placed over the exposed cord, and sutured to the
cut edges of the dural membrane surrounding the cord.
Because creating the omental pedicle can be tricky,
some surgeons use a substitute procedure, in which a free, unattached
piece of omental tissue is surgically placed over the injured cord and
connected to a surrounding vascular source (e.g., to the carotid artery
and jugular vein). Dr. Hernando Rafael in Mexico has mostly used this
modified procedure to treat over 250 people with spinal cord injury.
Although blood circulation is maintained, because the graft is separated
from the omentum’s lymphatic system, the tissue’s ability to absorb
fluid is eliminated.
IMPROVEMENT
RATE:
Goldsmith and Rafael estimate that about 40% of
their omental SCI patients have regained some function, and Chinese
surgeons have reported an even greater improvement rate.
Critics tend to dismiss such claims, however,
because they are often based on subjective evaluation criteria affected
by potential doctor or patient biases. These critics believe that
improvement can only be documented through validated clinical outcome
measures to assess patient function before and after treatment.
In response, advocates believe that restored
function is often so great that efficacy cannot be denied. One omental
patient noted that his extensive improvement after omental surgery was
dismissed by the physician he had been seeing as merely recovery from
hysterical paralysis - even though the improvement was five years after
his injury.
ANIMAL
RESEARCH:
Since 1975 when Goldsmith first demonstrated that
placing the omentum on the injured spinal cord in dogs could
revascularize the underlying cord tissue, many animal studies have shown
omentum’s therapeutic potential.
For example, numerous projects have evaluated the tissue’s
ability to treat a contusion injury that produces a cavity in the cord
similar to many injuries in people.
This research indicated that placing an omental pedicle on the
injury area will inhibit cavity formation and preserve overall function.
Research in cats has also shown that the omentum
can even help repair a totally transected spinal cord. In this research,
the gap in the cord was filled with liquid collagen, such as used in
cosmetic surgery, that hardens at body temperature. The omental pedicle
was then placed over this collagen bridge that formed between the spinal
cord stumps.
Compared to control cats, spinal cord blood flow
was greatly increased across the omentum-collagen bridge. More
importantly, neuronal axons grew through the bridge into the cord on the
other side of the gap (see illustration) at a rate of one millimeter per
day. This rate is comparable to peripheral nerve regeneration (i.e., the
nerves outside of the brain or spinal cord that usually retain
regeneration capability). The procedure prevented hind-limb muscle
atrophy, and as recorded on video, even allowed some cats to regain
coordinated walking ability.
OMENTAL
SURGERY IN PEOPLE:
In 1984, Goldsmith carried out the first surgery in
a person with spinal cord injury (see below). Although many people with
SCI have had omental surgery since that time, a 1996 study (Clifton, et
al, Spinal Cord, 34, 1996)
appeared to provide the scientific ammunition to dismiss the procedure
as a viable SCI treatment.
In this study, 11 patients with spinal cord injury
were examined a year after omental surgery using a variety of
state-of-the-art assessment procedures and compared to control subjects.
The overall results were inconclusive; some subjects appeared to
improve, and others did not. Because these ambiguous results were
associated with some serious side effects, the investigators concluded
that there was “ no justification for further clinical trials of this
procedure.”
For most of us in the SCI research establishment,
because the study used the correct assessments, it seemed to be the
final nail in the coffin for the therapy. However, like newspaper errata
that are rarely noticed, few saw Goldsmith’s rebuttal that was
published soon after (Spinal Cord,
35, 1997).
Goldsmith claimed that the study’s statistically
meaningless conclusions merely reflected the investigator’s existing
biases against the procedure. He noted that the investigators had used
two different surgical procedures, automatically confounding the study.
Over half the time, they had used a free omental tissue graft instead
of, as stated in their objectives, an attached omental pedicle. By so
doing, they eliminated the tissue’s beneficial fluid-absorbing
capability.
Although the study’s goal was to determine the
specific effect of the omentum placed directly on the injured cord, the
final analysis included outcomes of several patients whose omental graft
was shown not even to be physically attached to the cord or had been
surgically removed before analysis. In other words, they had factored in
results that were not applicable to the stated study objectives, and,
hence, significantly skewed the reported results.
A TREATMENT
FOR ACUTE SCI?
Although to date omental surgery has been
exclusively directed to long-term chronic injuries, based on animal
studies, Goldsmith believes that the procedure may be able to reduce the
extensive secondary neurological damage that occurs soon after injury. The swelling that develops after injury in and around the
cord can cut off capillary blood flow, which may prevent therapeutic
drugs from reaching the injury site, and creates the scar tissue that
that inhibits regenerative processes. Goldsmith says that the
spinal-column-stabilizing surgery (i.e., fusion) often carried out after
injury is a golden opportunity to reduce the damaging fluid edema by
placing the enormously absorptive omentum upon the injured cord.
CASES:
In addition to Sternberg, the individuals I talked
to were enthusiastic about the benefits they had accrued after omental
surgery, although they emphasized that one must have realistic
expectations.
In 1984, Daren Renna became the first person with a
spinal cord injury to be treated by Goldsmith. Several years earlier, as
a 17-year old, up-and-coming gymnast who was setting his sights on
qualifying for the U.S. Olympic team, Renna had become a C3-4
quadriplegic from a gymnastics accident.
His injury resulted in the loss of virtually all function below
the neck except for being able to rotate his hands slightly.
Renna says he has benefited greatly from omental
surgery.
“I initially got more balance and had less
spasticity. And over the next five years, I regained a lot of arm and
wrist function,” he says. “I have pretty good use of my arms now.
Overall, I am a much healthier person.”
Goldsmith was moved when Renna later gave him a
gymnastics medal in gratitude. Renna has become involved in gymnastics
again as a coach and internationally rated official (see photo).
In 1993, Andrea Zobell, a 23-year old German woman,
became paraplegic after a skiing accident. An MRI indicated a near total
transection of her spinal cord. Although retaining occasional lower leg,
light-touch sensitivity, she lost all physical movement below the T6-7
level.
More than three years later, Zobell had omental
surgery in which the scar tissue that now filled the 1.6-inch gap in her
cord was replaced with an omental-collagen bridge as described above.
After recovering from the surgery, she zealously committed to a physical
rehabilitation program, which she strongly believes is needed to
maximize surgical benefits.
Over the next several years, Zobell gradually
gained strength and control of muscles below the injury, Because of
increased strength in the back, hip, and abdominal muscles, she could
now remain in a sitting position without support. She has regained some
ability to move her legs. For example, she can walk when she is in a
swimming pool and can get off a chair and stand with some support (see
photo). She also has increased awareness of bladder filling.
Andrea’s MRI now shows the continued development of structure
connecting the spinal cord segments.
CONCLUSION:
There is too much supporting research and patient
experience to continue to ignore omentum’s therapeutic potential. The
verdict is not in for this procedure as many of us falsely concluded in
the past. We need to open-mindedly gather more evidence, especially
well-designed, controlled clinical trials to help definitively determine
the procedure’s benefits relative to its risks.
Adapted from “Paraplegia News” March 2001 (For
subscriptions, contact www.pn-magazine.com).