
See laserpuncture overview and
philosophy.
ABSTRACT:
Restructuring of Limb Morphology by Laserponcture®
Therapy and Preliminary Research to Understand its Mechanism of Action on
Muscle Activity in Patients with Spinal Cord Injury: Prospective Clinical
Study of 22 patients with Spinal Cord Injury, who Underwent laserponcture®
Treatment.
Objective: To show the action of the
laserponcture® technique on the morphology of skeletal muscles in spinal
cord injuries.
Setting: Clinic of Albert Bohbot, La Chapelle
Montlinard, France. Statistical study, Health Department, Faculté de
Médecine de Dijon, France.
Results: The effects of laserponcture
therapy on the limb morphology of 22 individuals with SCI (14 with
paraplegia and 8 with quadriplegia) were evaluated over time. Although
limb circumference increased over time in response to the therapy, the
evolution of this growth often varied between limbs. Specifically, these
variations indicate that growth of the right and left limb does not
progress at the same rate, but, nevertheless, tends to balance over time.
Conclusion: In the case of SCI, the study
results suggest that laserponcture® treatment promotes functional
restructuring of skeletal muscles.
Preamble:
Treated individuals were informed of study objectives.
INTRODUCTION:
During the last ten years, studies have documented
early alterations in skeletal muscles after spinal cord injury (SCI)
through the histological analysis of skeletal muscle biopsies. These
alterations are caused by the muscle functional disability such as disuse,
hypotonia, spasticity or micro-vascular damages, resulting in skin
pressure sores or ulcers. These disorders contribute to morphological and
histological alterations such as (1, 2, 3, 4, 5, 6):
1. Muscle atrophy with reduction of the skeletal
fiber diameter;
2. Vasodilatation of capillaries and interstitial
vasogenic edema;
3. Shift of the striated histochemical muscle fibers
of type I – located in deep muscles and the central part of superficial
muscles, whose contraction is low and sustained, and vascularization is
rich – to the striated histochemical muscle fibers of type II – located in
the peripheral part of superficial muscles, whose contraction is strong,
fast and short, and vascularization is poor;
4. Increase of the interstitial conjunctive tissues,
fatty infiltration, endomysial fibrosis and microangiopathy.
The time that has elapsed since injury has an
influence on the muscle fiber diameter.
In certain cases of disuse, combining transcutaneous
electrostimulation with intensive physiotherapy modifies the morphological
profile, increases muscle capillaries, and reverses muscle fiber
alteration, all revealed by the biopsy. But these improvements are
temporary and do not take part in the ability of doing and repeating a
voluntary act, and controlling the muscle contraction (4, 5, 6).
Electrostimulation tires the paralyzed muscle four times quicker than the
non-paralyzed fiber and may damage the muscle fiber because of electrical
saturation (4, 5, 7).
Considering these factors, we speculate on the
effects of biophotonic laserponcture® therapy on paralyzed muscle
morphology after SCI (biophotonic acts as a go-between in the relations
between photon – fundamental element of light – and the different
biological layers that makes the cell molecules, the cells, the tissues
and organs). Contrary to transcutaneous electrostimulation (which is an
application in physics of an electrical phenomenon that triggers and
controls the contractions of the underlying muscle without the
individual’s will), this therapy is applied on the body (the laser head is
laid on the skin) and expresses its effects inside the body (coherent
light which runs through the classic acupunctural network and Bohbot’s
neo-acupunctural network (BNA) used for laserponcture® (11, 12)), taken
over by the brain.
To determine whether laserponcture® therapy increases
skeletal muscle size below the injury, we undertook a prospective clinical
study measuring lower-limb circumference in 22 patients with SCI (14 with
paraplegia and 8 with quadriplegia) treated by laserponcture®.
MATERIALS & METHODS:
Laserponcture® is a unique therapeutic process
initially developed by Albert Bohbot in 1979 (8, 9, 10, 11, 13, 14).
The device is a multi-frequency infrared laser beam.
In over 30 years of use, few side-effects have been reported (10, 11, 15).
With support by a French government grant, this laser
machine was developed according to specific specifications by the Ecole
Nationale Supérieure des Arts et Métiers (ENSAM), Cluny, France.
The range of frequencies can be adjusted hertz by
hertz with this laser device and
computer-piloted by a program with a specific microprocessor. Because of
the device’s proprietary status, its intrinsic parameters cannot be
disclosed in this article.
Laserponcture® is one of many therapeutic
applications of low-power laser devices in humans. So far, the low-power
lasers in neurological applications are used for the research in vivo on
the peripheral nerves of brain cells or embryonic cells in rats (3, 16,
17, 18, 19, 20). Numerous scientific or medical studies on lasers have
been published in the last years (15, 21, 22, 23, 24, 25, 26, 27,
28, 29).
The therapeutic process is based on a diffusion of
photons emitted by the laserponcture® machine in the energy physiology
within the classic acupunctural and Bohbot’s neonetwork, which has 300 new
points. This new cartography is the result of 20 years of research on the
acupunctural network and ancient Chinese texts (30), which enabled Bohbot
to elucidate the location of new points. In the Synthèse des travaux
des symposia de Pékin, 15 juin 1979 (31), it is specified that on
average a new point is discovered every year, complementing the classic
acupunctural network. In the case of SCI, this therapeutic principle is
completed by the stimulation of cutaneous dermatomes, which results in a
criss-cross matrix carrying the energy: horizontally, dermatomes match the
spinal cord segments cutaneously; and vertically, the classic acupunctural
network is completed by BNA cartography (8, 9, 32).
The laser head is applied on the skin, which acts as
a mediator between the laser emission and the underlying channel network
located in the hypodermic area. It constitutes the histological and
biological border between the outside and inside world (8).
In each session, the same therapist applied the laser
head from the same device to eight different cutaneous points
successively. Specifically, the laser head was applied to points on the
upper part of the body, back or front alternately. Each point was
stimulated for two minutes.
The statistical study was carried out in a blinded
fashion at the Health Department of the Centre Hospitalo-Universitaire in
Dijon, France.
The study specifically consisted of observing the
evolution of lower-limb circumference (in centimeters) in 22 patients with
SCI. It is a prospective, observational clinical study realized at the
patient’s bed.
Patient description: Only individuals with SCI
took part in the study:
The lower limbs measurements were always taken by the
same examiner using the same meter. The therapist, examiner, and
statistician were three different persons. Specific anatomic areas of the
lower limbs were taken to measure the limbs circumferences:
Thighs: 15 cm above the upper edge of the
patella.
Legs: 10 and 15 cm below the lower edge of the
patella.
This 21-month study was done between 1 January 2001
and 30 September 2002. The program combined one laserponcture® session
with rehabilitation exercises on a daily basis (standing-frame, electric
bike, stationary bike, muscle bench and walk in parallel bars with
knee-ankle-foot orthosis articulated at the knee and ankle level).
The first measurement was taken during the first
visit. Each patient had at least four measurements.
The treatment frequency varied due to the travel time
from the clinic to the patient’s residence. It could vary from one session
a day during three consecutive months to one session a day during one week
every eight weeks.
Descriptive statistical analyses were carried out in
a blinded fashion. The measurements, expressed in percentage for each
individual, were recorded over time. The system of reference “0”
corresponds to the first measurement. The first variations, which appear
at three months on the graph, correspond to the average of the variations
observed between one and three months for each patient. The mechanism of
calculation is the same for 6, 12 and 18 months.
The curve represents the median of these variations
for all the individuals.
RESULTS:
The analysis shows that the right and left limbs do
not change at the same time and at the same speed, but tend to balance
each other.
1. The muscle volume
of a limb can increase quicker than the other. It can be noticed that
after the curves met, the tendency can be reversed and the limb, which was
behind, can then increase quicker.
2. The two curves meet in the three graphs at 6, 12
and 18 months. This phenomenon begins towards the fifth month of treatment
with the calves measured at 15 cm, i.e. the remotest measurement from the
navel; then it evolves towards proximity with the calves measured at 10 cm
towards the sixth month; and finally, the thighs towards the seventh month
of laserponcture® therapy. Then, the curves of the lower limbs meet with a
periodicity of six months on the three graphs.
The circumference of the calf measured at 15 cm
evolves at its own pace of three months, which is faster than the calf and
thighs measured at 10 cm. However, this variation alternates between rises
and falls, and somewhat a global stability in measurements.
2) Median curve of the variations of the calf circumference measured at 10
cm over time in patients with SCI and treated by laserpuncture.
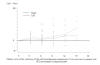
3) Median curve of the variations of the calf circumferences measure at 15
cm over time in patients with SCI and treated by laserpuncture.

*Authors:
Albert Bohbot,
state-registered podiatrist, director and founder,
Laboratoire de recherche sur le laserponcture®, independent researcher in
neurosciences. Address: Château Gaillard – 33 route du canal – 18140
La Chapelle Montlinard – France – Phone and
fax (work): +33 2 48 79 43 61 – Phone (home): +33 2 48 79 47 09 – Email: albert@laserponcture.net.
Practitioner of laserponcture®.
Cécile Jame-Collet,
MD, Traditional Chinese Medicine, Faculté de Médecine de Paris Nord.
Address: Chérault – 58270 Saint-Benin-d’Azy – France – Phone:
+33 3 86 58 45 18 – Email:
cecile.jcollet@wanadoo.fr.
Observer in charge of taking measurements.