
The 3rd annual meeting of the
International Association of Neurorestoratolgy (IANR) was held April
23-25th in Beijing, China. Attended by scientists from
throughout the world, the conference’s overall goal was to open-mindedly
bring together divergent perspectives in an effort to accelerate the
development of real-world therapies for a variety of neurological
disorders, including SCI, amyotrophic lateral sclerosis (ALS), stroke,
and Alzheimer’s, Parkinson’s, and Huntington’s disease. .jpg)
Neurorestoratology is an emerging
neuroscience subdiscipline that emphasizes regeneration or repair of the
damaged nervous system. Its objective is the recovery of neural function
lost due to trauma, neurodegenerative disorders/diseases, compromised
blood flow, etc. Although many therapeutic strategies fall under the
neurorestoratology umbrella, a key focal point has been stem-cell
transplantation.
Believing that return of some life-enhancing
function for many, once considered untreatable, disorders is now within
our reach, the IANR’s mission is to speed up the bench-to-bedside
transition of basic-science laboratory research into beneficial clinical
therapies, in part, by pulling together the divergent pieces of the
puzzle emerging throughout the world.
Recognizing that SCI bows to no flag, the IANR
believes its goals can be achieved through fostering better
communication between world scientists. Indeed, I thought that one of
the conference’s greatest strengths was the opportunity to interact with
scientists from Russia, China, etc who often possessed a different view
on how to do things from many of my US colleagues.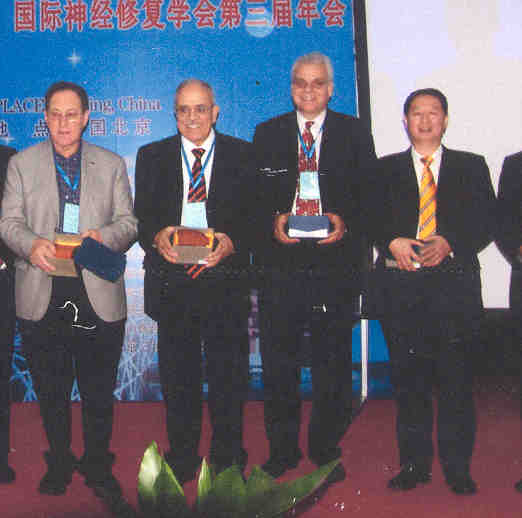
The driving force behind the IANR’s creation was
China’s Dr. Hongyun Huang a pioneer in developing
function-restoring, cell-transplantation procedures. Several senior
scientists from throughout the world have assisted him in his IANR
organizational efforts, including 1) England’s Dr. Geoffrey Raisman,
whose animal research laid the foundation for Huang’s procedures, 2)
Dr. Paul Sanberg, University of South Florida, one of America’s
foremost stem-cell experts, and 3) Dr. Ziad Mohammed Al-Zoubi,
President of the Pan Arab Spine Society and organizer of next year’s
conference in Jordan. (photo: Drs. Raisman, Al-Zoubi, Sanberg & Huang)
Sample Presentations
Conference organizer Dr. Huang proved a
big-picture overview of the nascent field of neurorestoratology,
including some of the cell-transplantation programs emerging throughout
the world, as well as key issues concerning and limiting their
development. Although we have a long way to go before there is a true
SCI cure, he emphasized neurorestoratology is bearing fruit now by
providing some life-enhancing functional improvements.
Huang stressed that the needs of patients to have
access to potentially beneficial therapies in a timely fashion should be
given greater priority. As such, we should more expeditiously and
effectively translate basic-science discoveries into real-world clinical
applications. Although ensuring scientific purity, our allegiance to an
exacting scientific process often creates insurmountable barriers in
getting treatments to patients. Underscoring his belief, Huang quoted
the 2000 Declaration of Helsinki (a policy delineating medical
ethical principles):
“In the treatment of a
patient, where proven prophylactic, diagnostic and therapeutic methods
do not exist or have been ineffective, the physician, with informed
consent from the patient, must be free to use unproven or new
prophylactic, diagnostic and therapeutic measures, if in the physician's
judgment it offers hope of saving life, reestablishing health or
alleviating suffering.”
Dr. Paul Sanberg (Florida) provided an
overview of his stem-cell research focused on treating stoke and other
neurological disorders. He suggested that aging, itself, with its
decline in regenerative ability represents a stem-cell disease. With
age, there is a diminution in number of stem cells and their potency. In
this regard, Sanberg noted that one promising advance is the development
of biopharmaceuticals that stimulate or help maintain our body’s
stem-cell robustness as we age.
Because of the difficulty in the US of using
theoretically powerful, but controversial embryonic stem cells, Sanberg
focused his efforts on transforming uncontroversial, bone-marrow-derived
stem cells into neural progenitor cells for treatment of neurological
disorders. Because readily available umbilical cord blood is a good
source of bone-marrow-derived stem cells, he used it for his research.
Animal studies suggest that these umbilical stem
cells can, indeed, differentiate into neuronal stem cells with
reparative potential in stroke. Injected intravenously, the cells appear
to migrate to where they are needed and induce some behavioral recovery.
In an example of our need to pull together the puzzle pieces, Sanberg
noted that certain drugs enhance the overall effectiveness of the
transplanted stem cells. Given such findings, it is likely that many
future stem-cell therapies will be combined with an augmentative drug
treatment. Indeed, this is the case for an ongoing SCI-focused clinical
trial, which combines umbilical stem-cell transplantation with lithium,
a neuroprotective agent.
Sanberg also underscored that the time of stem-cell
administration after neurological insult is a key consideration. If the
cells are transplanted too early or late, efficacy will be compromised.
He believes this is a good example of why we need a strong base of
animal research before transitioning to humans.
Sanberg concluded with a thought-provoking
discussion on the potential downside associated with the increasingly
popular practice of quickly cutting and freezing the umbilical cord for
future therapeutic needs. Specifically, if cord cutting is delayed,
stem-cell-rich cord blood will be pumped into the newborn. Studies
suggest that this infusion enhances infant health. Sanberg noted that
mankind has become the only species not allowing the transfer of cord
blood into its newborns, which may have long-term, adverse consequences,
especially for preterm infants. He ended with the observation that women
in ancient cultures often gave birth while squatting, allowing the cord
blood to flow into the newborn due to gravity. So to speak, umbilical
cord blood was “mankind’s first transplant.”
Dr. Adeeb Al-Zoubi (Jordan), founder,
Stem Cells of Arabia Network and his colleagues have transplanted
bone-marrow-derived, purified stem cells into ~50 patients with SCI.
Isolated from the patient’s bone marrow (hence, minimal rejection
potential), these cells were reintroduced into the patient’s spinal
cord. Although some improvements were noted, he believes the results are
“suboptimal.” As such, Al-Zoubi is researching ways to better prepare,
process, and differentiate these and other bone-marrow-derived cells
into more neurologically oriented stem cells with, in turn, a greater
potential to treat neurological disorders.
In reviewing various stem-cell programs emerging
throughout the world, Al-Zoubi has observed that programs can be broadly
assigned to three different operating models:
1) With the classical
scientific model, progress is slow and proceeds carefully, results
are well reviewed and criticized by peers, and strong publications are
produced. Usually, the major financial benefits accrue to biotech/drug
companies not the scientist.
2) The opposite extreme is
the aggressive model, in which there is little scientific basis,
results are unknown, there is an absence of publications; but the
program is a moneymaker.
3) The progressive
model is between these two extremes. Although it takes advantage of
the scientific process, it moves quickly to a patient-oriented
disease/disorder-treating emphasis. However, because it generates a
weaker foundation of publications, the program is often criticized.
Dr. Andrey Bryukhovetskiy is the director of
Moscow’s stem-cell focused NeuroVita
Clinic, as well as former Chief Neurologist, Russian Navy. (Photo:
Dr. Bryukhovetskiy & author) His
presentation focused on the epigenetic reprogramming of stem
cells to increase their potential for treating neurological disorders.
Basically, under epigenetic principles, we are not merely a hardwired
manifestation of our genetic DNA as once thought. The genes we express
and, as a result, who we become is influenced by diverse environmental
factors.
His
presentation focused on the epigenetic reprogramming of stem
cells to increase their potential for treating neurological disorders.
Basically, under epigenetic principles, we are not merely a hardwired
manifestation of our genetic DNA as once thought. The genes we express
and, as a result, who we become is influenced by diverse environmental
factors.
As discussed by Bryukhovetskiy, this epigenetic
concept has great relevance for the development of stem-cell therapies.
Basically, his overall goal is to epigenetically manipulate such cells
to turn them into more regeneratively robust cells better tailored to
treat specific neurological disorders. As part of his efforts,
Bryukhovetskiy encapsulates growth-influencing factors within tiny
biodegradable nanocapsules. These will be incorporated into the stem
cells isolated from the patient. After transplantation back into the
patient, the nanocapsule-containing stem cells will migrate to the
dysfunctional area. Eventually, the nanocapsules will biodegrade
releasing the growth-influencing factors. Depending upon their specific
nature, these factors should steer the neighboring dysfunctional tissue
in the desired direction, e.g., perhaps regeneration or, in the case of
tumors, cell death.
Laser Therapy: Energy-based therapies
represent another intriguing piece of the restoration puzzle. For
example, numerous studies suggest that laser therapy has a
neuroprotective effect, preserves injured nerve functional activity,
decreases injury-site scar tissue, lessens degeneration in corresponding
motor neurons of the spinal cord, and increases axonal growth and
insulating myelin.
Developed by France’s Albert Bohbot,Laserpuncture
combines elements of laser therapy and acupuncture, both of which
influence the expression of regenerative stem cells.
.jpg)
A number of stem-cell
recipients with SCI have attempted to maximize restored
post-transplantation function with Laserpuncture. Bohbot’s presentation
specifically focused on the improvements, as measured by
electromyography (electrical recording of muscle activity), of three
individuals who underwent Huang’s cell-transplantation procedures. Huang
uses olfactory-derived cells that have been shown to promote
axonal regeneration by 1) producing insulating myelin sheaths around
both growing and damaged axons, 2) secreting growth factors, and 3)
generating structural and matrix macromolecules that lay the tracks for
axonal elongation. Bohbot’s results suggest
that the Laserpuncture/cell-transplantation-combination therapy restored
some voluntary muscle activity. This is a good example of the sort of
pulling-together-of-the-pieces effort we need.
SCI Resource:
I provided an overview of an extensive database that I’ve created
of diverse therapies that have the potential to restore some function
after SCI. Developed with the patronage of
the Iceland’s Institute of Spinal Cord Injury, the
information has been posted in five languages on
www.sci-therapies.info (English, Spanish, Chinese, Russian, and
Arabic). In addition, PVA has tentatively agreed to publish the
database as a book. The foreword to this resource was written by former
Iceland President Vigdis Finnbogadottir (sidebar). In addition to
defining the project in a all-inclusive fashion that resonates with the
IANR goals and objectives, she placed its mission within a human-rights
context.