
The 4th
International Symposium on Experimental Spinal Cord Repair and
Regeneration took place March 25 – 27, 2002 in Brescia, Italy, about
50 miles east of Milan between the Italian Alps foothills and the Po
Plain.
The University of
Brescia’s Professor Giorgio Brunelli, a preeminent spinal cord injury
(SCI) surgeon, organized the symposium and extended much culturally
imbued hospitality to the participants. For example, celebrated soprano
Katia Ricciarelli presented a memorable operatic concert. 
Approximately 40
speakers from Europe and North America offered a multidisciplinary
diversity of SCI research and therapeutic approaches, ranging from basic
neuroscience to innovative surgical procedures. Due to space
constraints, this article summarizes only a few highlights.
Nerve Growth Factor:
The symposium emphasized the contributions of many
Italian scientists, including Dr. Rita Levi-Montalcini, the 1986 Nobel
Laureate in medicine. While working at St. Louis’ Washington
University 50 years ago, Levi-Montalcini discovered nerve growth factor,
one of the 20th century’s major neurobiological
breakthroughs. The discovery has not only profoundly influenced
today’s SCI research but also helped undercut the then-axiomatic
assumption that regeneration after SCI was impossible. Her insightful
remarks and engaging personality indicated no lack of this nerve growth
factor in spite of being 93.
Clinical Trials Update:
Dr. Wise Young (Piscataway, NJ) provided an
overview of an ever-growing number of promising SCI interventions,
including those that have entered the clinical-trial evaluation process.
Among these procedures are the use of various neuronal growth factors
that have been discovered since Levi-Montalcini’s initial
breakthrough; alternating electrical currents; antibody blockers of
inhibitors that prevent regeneration; various remyelination and
4-aminopyridine-facilitated approaches that enhance conduction;
transplanted stem cells that can transform into new neuronal cells;
immunological approaches; and etc. (see http://carecure.rutgers.edu,
clicking on CareCure Community for more detailed summaries).
Immunological Approaches:
Dr. Michal Schwartz (Rehovot, Israel), scientific
founder of Proneuron, an SCI-focused biotechnology company, discussed
immunological approaches that minimize neurological damage after injury.
Inspired by Hippocrates’ ancient wisdom that “natural forces within
us are the true healers of disease,” Schwartz uses the body’s
inherent healing mechanisms to develop therapeutic approaches that
proactively augment naturally occurring autoimmune processes. These
approaches use the patients’ own immune cells (called macrophages and
T-lymphocytes), to minimize post-injury secondary damage and promote
neuronal regeneration.
Although immune cells are scarce in
“immune-privileged” central nervous system (CNS) tissue, to a
limited degree they accumulate at the injury site, providing some
neuroprotective and neuroregenerative potential. Schwartz manipulates
this autoimmune response to greatly boost its healing potential.
Patients in the acute injury phase have been
recruited for Proneuron-sponsored phase-one clinical trials by (see www.proneuron.com).
As a result of Schwartz’ research, future SCI healthcare may
see patients receiving a damage-reducing, regeneration-promoting
vaccination after injury. As a consequence, the SCI pipeline may be
further closing at the source.
Rerouted Nerves:
Professor Brunelli, the symposium’s organizer, is
pioneering promising surgical procedures for restoring function after
SCI. Specifically, he is one of the first to surgically reroute
peripheral nerves (i.e., those outside of the spinal cord and brain) to
bypass the injury site, reestablishing a functional neuronal connection
from the brain to previously dormant body areas (see PN April,
2002 & September 2001).
Building on much animal research, Brunelli has
developed several rerouting variations to restore some function in
patients with SCI. In the first, he redirected and connected the
wrist’s ulnar nerve, which emanates above the injury site, to nerves
that control leg muscle functioning below the injury site.
In the second variation, Brunelli has used the
peroneal nerve (a nerve to the leg that emanates below the injury site)
as a bridge from the spinal cord above the injury site to the nerves of
the gluteus and quadriceps muscles, obtaining a direct connection of CNS
with these leg muscles.
The former procedure provoked less controversy
because it involves connecting two peripheral nerves, which due to their
inherent regenerative potential increases the likelihood of functional
connections. Because the latter procedure involves establishing
more-difficult connections between the spinal cord and peripheral
neurons, some scientists felt that additional documentation (e.g., gene
studies), were necessary before the observed restored function could be
attributed to this specific intervention. Since the upper motor neuron
(nerves within the spinal cord controlling movement) and lower motor
neurons (nerves that leave the cord to connect to muscles) use different
neurotransmitters (a chemical released from a neuron ending that
interacts with an adjacent neuron or muscle cell), gene research should
provide more definitive information on the mechanism of action of this
function-restoring procedure.
Scar Reduction:
Dr. Susanne Hermanns (Dusseldorf, Germany)
discussed biochemical interventions that make the post-injury scar more
permeable to neuronal axons attempting to regrow through the injury
site. Using rats, Hermanns has shown that these interventions can
inhibit the biosynthesis and deposition at the injury site of collagen,
a key component of scar tissue. This creates a more permissive
environment for transected axons to migrate through the injury site.
Olfactory Ensheathing Cells:
Dr. Susan Barnett (Glasgow, UK) reviewed research
on transplanting olfactory ensheathing cells (OEC’s) into the injury
site. OEC’s are specialized glial cells (i.e., those that provide
physical and metabolic support for neurons) associated with olfactory
system neurons. Unlike other CNS neurons, these neurons have
considerable re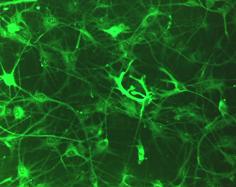 generative
ability due to OEC production of new insulating myelin sheaths around
axons and promotion of axonal regrowth.
generative
ability due to OEC production of new insulating myelin sheaths around
axons and promotion of axonal regrowth.
OEC’s also have considerable
regeneration-promoting properties when transplanted into the SCI injury
site. Not only to they remyelinate and promote regeneration of SCI
transected axons, but studies suggest OEC’s can restore some
functional recovery. For example, Dr. Patrick Gauthier (Marseilles,
France) discussed how OEC transplantation into the traumatic high
cervical injury site could restore respiratory function in rats.
It’s the Blood Supply!
Dr. Henry Crock (London, UK) provided an overview
of the paramount, yet often under-appreciated, role of the spinal
cord’s blood supply. He
reminded the audience how important this supply was in nurturing the
neurons that we are struggling to regenerate.
“Don’t throw away the walking stick of spinal
injury,” Crock noted, emphasizing that both arterial and venous cord
circulation is the primary thing that needs to be addressed in SCI.
For example, in post-injury SCI management, Crock
stressed that surgeons must be careful in spinal stabilization so as not
to aggravate paralysis through compromising existing blood supply.
Furthermore, he suggested that our research efforts to develop new
therapies might be more productive if emphasis was placed on mechanisms
that would increase spinal-cord blood circulation.
Several other speakers noted such
circulation-promoting mechanisms in their talks.
For example, Dr. Harry Goldsmith’s (Reno, Nev.) omental
transposition procedure - in which the gut’s highly vascularized
omental tissue is surgically transposed to the injury site - exerts its
restorative effects partially through stimulating new blood vessels into
the spinal cord region (see PN, March 2001).
While discussing Eastern-healing therapies, Dr.
Laurance Johnston (Boulder, Colo.) noted how acupuncture is hypothesized
to restore function after SCI through improving circulation around the
cord (see PN, September, 1998).
Also consistent with this theme, Dr. Weihong
Pan’s (New Orleans) research focused on the changes in the blood
spinal-cord barrier (BSCB) that occurs after injury. The extra tight
cellular junctions that exist in CNS-associated capillaries create the
BSCB, which inhibits large molecules from passing from the blood into
the cerebrospinal fluid.
By studying the uptake of an immunological molecule
that exerts regenerative effects at low concentrations, Pan has shown
that post-injury BSCB disruption is reversible and varies depending upon
the affected spinal region. Her studies suggest that the dynamic
regulation of BSCB could play a pivotal role in spinal cord
regeneration.
Functional Electrical Stimulation (FES):
Many speakers focused on the use of various forms
of FES to stimulate paralyzed muscles. From the US, Drs. Michael Keith
and Harry Hoyen (Cleveland, Ohio) reviewed their efforts to develop
increasingly technologically sophisticated and physiologically
integrated FES neuroprostheses for restoring hand and upper-arm
function.
European scientists have especially embraced
diverse FES applications as part of their rehabilitation and research
programs. For example, Dr. Hans Van der Aa, (Enschede, Netherlands),
discussed the long-term effectiveness of the implanted Brindley device,
which stimulates paralysis-affected, bladder-controlling sacral nerve
roots.
In another example, Dr. Fin Biering-Sorensen
(Copenhagen, Denmark) discussed the results of a multi-institutional
European study, examining the effects of FES on individuals with
incomplete SCI. Although no increase in walking endurance was found, FES
training enhanced gait and overall walking quality. Biering-Sorensen
also reported that FES cycling for 30 minutes three times a week over a
year increased bone density by 10%. However, if the cycling session was,
in turn, reduced to once a week, the regained density was lost.
Conclusion:
Celebrated science-fiction author Arthur C. Clarke
has stated “When a
scientist states that something is possible, he is almost certainly
right; when he states that something is impossible, he is very probably
wrong.“
Given Clarke’s observation, the growing optimism
that was percolating to the surface in-spite of the speakers’ inherent
conservative nature portends much promise for the future.
Adapted from article appearing in Paraplegia News, August, 2002 (For subscriptions, contact www.pn-magazine.com).